Signs, symptoms, and diagnosis
Signs and symptoms are often mild. Nowadays, people with hemochromatosis are less likely to develop symptoms, as diagnosis tends to happen earlier than it did in the past.
If the condition advances, the main symptoms include:
- Abdominal pain
- Females may stop menstruating
- High blood sugar levels
- Hypothyroidism, or low thyroid function
- Loss of libido, or sex drive, and male impotence
- Reduction in size of testicles
- Skin becomes bronzed, like a suntan
- Tiredness or fatigue
- Weakness
- Weight loss
In time, the following conditions may develop:
- Arthritis
- Cirrhosis of the liver
- Diabetes
- Enlargement of the liver
- Heart disease
- Pancreatitis
Around 75 percent of patients who have started to show symptoms will have abnormal liver function, 75 percent will experience tiredness and lethargy, and 44 percent will have pain in the joints. A bronze skin color will be visible in 70 percent of patients with symptoms.
Risk factors and causes
There are some known risk factors for hemochromatosis.
Genetic factors: Having two copies of a mutated “high iron” or, HFE gene, is the greatest risk factor for hereditary hemochromatosis. The person inherits one copy of the mutated HFE gene from each parent. H refers to high, and FE means iron.
Family history: A person with a parent, child, brother, or sister with hemochromatosis is more likely to have it.
Ethnicity: People of British, Scandinavian, Dutch, German, Irish, and French ancestry have a higher risk of having the HFE gene mutation and of developing hemochromatosis.
Gender: Men are significantly more likely to develop hemochromatosis than women, and they tend to experience signs and symptoms between the ages of 40 and 60 years, while women are more likely to develop it after menopause.
This is because women lose iron during menstruation and pregnancy. A woman’s risk increases after the menopause or a hysterectomy. Among every 28 people with hemochromatosis, 18 are male and 10 are female.
Some researchers have suggested that genetic hemochromatosis may be linked to autoimmune thyroiditis, either playing a role in the development of thyroiditis, or overlapping with it.
Causes
Most people absorb around 10 percent of the iron they consume. When there are sufficient stores of iron, the body reduces iron absorption through the intestine to prevent levels from rising too far.
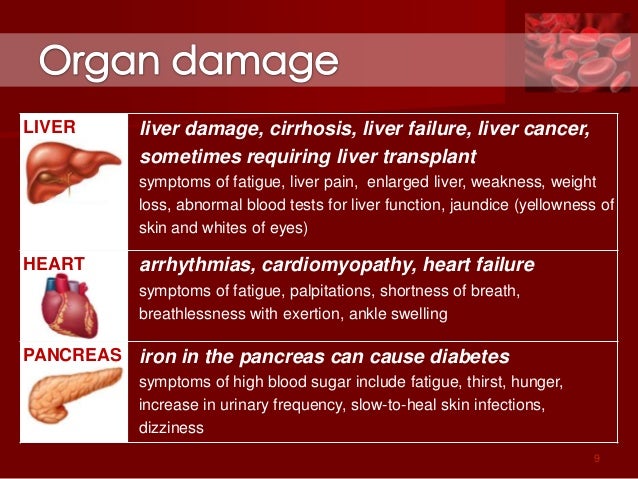
People with hereditary hemochromatosis may absorb up to 30 percent of the iron they consume. At this rate, the body cannot expel the extra iron fast enough, so it builds up. The body stores the excess in the tissues of major organs, mainly in the liver, and also the heart and the pancreas.
People with hemochromatosis may eventually build up between 5 and 20 times the amount of iron they should have. Over time this excess iron can destroy organs, resulting in organ failure and chronic diseases, such as cirrhosis, heart disease, and diabetes.
Primary hemochromatosis: A genetic mutation
Every living organism has genes. Genes are a set of instructions that decide what the organism is like, how it survives, and how it behaves in its environment. A mutation in one gene can change the way the body works.
![[genetic test]](http://cdn1.medicalnewstoday.com/content/images/articles/166/166455/genetic-test.jpg)
Genetic tests can show whether a person is likely to develop hemochromatosis and enable an early diagnosis.
HFE is the gene that controls the amount of iron we absorb. The two common mutations in the HFE gene are C282Y and H63D. In the U.S., most people with inherited hemochromatosis have inherited two copies of C282Y, one from the mother and the other from the father. Around 31 percent of people with two copies of C282Y develop symptoms by their early fifties.
A person who inherits just one gene with the C282Y mutation is not certain to develop iron overload syndrome, although they will probably absorb more iron than normal, and they will be a carrier.
If both parents are carriers, there is a 1 in 4 chance of inheriting two mutated genes, one from each parent. However, some people with two copies of the C2H2Y mutation never experience symptoms.
Some individuals may inherit one C282Y and one H63D mutation. A small proportion of these people will develop hemochromatosis symptoms.
Inheriting two copies of H63D is rare. Having two copies of the H63D mutation may increase the risk of developing hemochromatosis, but this is not confirmed.
Men with HFE defects can develop symptoms from the age of 40, but in women, symptoms normally appear after the menopause.
Treatment and complications
Venesection, or phlebotomy, is a regular treatment to remove iron-rich blood from the body. It is like donating blood, but the aim is to reduce iron levels to normal.
How much blood is taken and how often depends on the patient’s age, overall health, and the severity of the iron overload. Normally, this happens weekly until levels return to normal.
When iron levels build up again, the patient will need to repeat the treatment.
Phlebotomy cannot reverse the symptoms of cirrhosis, but it can improve symptoms such as nausea, abdominal pain, and fatigue. It may improve heart function and joint pain.
The amount of blood that can be taken depends on whether the patient is male or female, and their overall health condition. One unit a week is normally taken. One unit is one pint or around 473 milliliters.
Medications can include a drug that binds the excess iron before being excreted from the body.
The patient should have regular blood tests, and treatment normally continues for life.
Life expectancy is normal if hemochromatosis is diagnosed and treated early, before too much additional iron accumulates.
Complications
If hemochromatosis is left untreated, the accumulation of iron can lead to complications.
These include:
- Cirrhosis, or permanent scarring of the liver, which can lead to serious and life-threatening complications
- A higher chance of liver cancer in individuals with both cirrhosis and hemochromatosis
- Diabetes and associated complications, such as kidney failure, blindness, and heart problems
- Congestive heart failure, if too much iron builds up in the heart and the body cannot circulate enough blood to meet its needs
- Irregular heart rhythms, or arrhythmias, leading to chest pain, palpitations and dizziness.
- Endocrine problems, such as hypothyroidism and hypogonadism
- Arthritis, osteoarthritis, and osteoporosis
- Bronze or gray skin color due to the deposits of iron in skin cells
Other complications can include depression, gall bladder disease, and some cancers. Autopsies have indicated that some people with neurodegenerative diseases, such as Alzheimer’s, have had high iron levels.
To reduce iron absorption, people with the condition have been encouraged to avoid red meat and other foods rich in iron, but reducing the intake of dietary iron has not been shown to lower iron levels. However, patients are advised not to take iron tablets or use vitamin C supplements, as vitamin C enhances iron absorption.
A high sugar consumption may also increase absorption of iron. Calcium-rich foods and eggs and tea may inhibit iron absorption.
People with the condition should limit the alcohol they drink, because it will increase the risk of liver damage.















![[Woman fainting]](http://cdn1.medicalnewstoday.com/content/images/articles/182/182524/woman-fainting.jpg)