Obstructive Sleep Apnea(OSA) is a sleep disorder that causes breathing to repeatedly stop and start during sleep.This occurs because of narrowed or blocked airways.
It is the most common type of sleep-disordered breathing and is characterized by recurrent episodes of upper airway collapse during sleep The disorder results in decreased oxygen in the blood and can briefly awaken sleepers throughout the night
It is the most common type of sleep-disordered breathing and is characterized by recurrent episodes of upper airway collapse during sleep
Signs and symptoms of obstructive sleep apnea include:
- Excessive daytime sleepiness
- Loud snoring
- Observed episodes of stopped breathing during sleep
- Abrupt awakenings accompanied by gasping or choking
- Awakening with a dry mouth or sore throat
- Morning headache
- Difficulty concentrating during the day
- Experiencing mood changes, such as depression or irritability
- High blood pressure
- Nighttime sweating
- Decreased libido
- If you have OSA, you usually begin snoring heavily soon after falling asleep.
The snoring often becomes very loud.Snoring is interrupted by a long silent period while your breathing stops.
The silence is followed by a loud snort and gasp, as you attempt to breathe.
This pattern repeats throughout the night.
Most people with OSA do not know their breathing starts and stops during the night. Usually, a sleep partner or other family members hear the loud snoring, gasping, and snorting. Snoring can be loud enough to hear through walls. Sometimes, people with OSA wake up gasping for air.
Causes
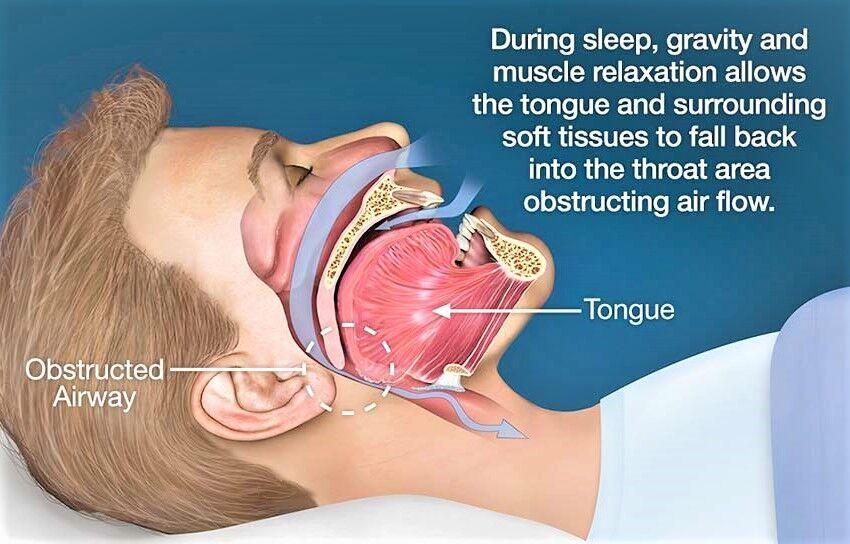
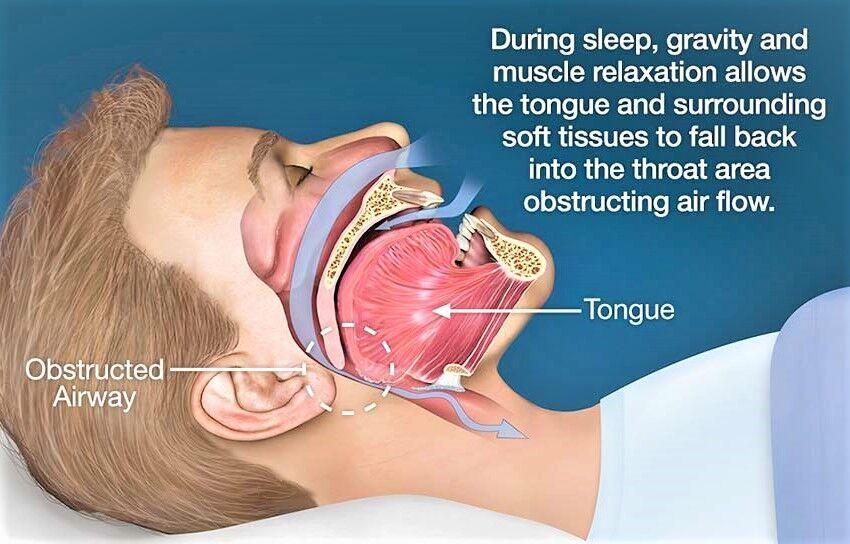
Obstructive sleep apnea occurs when the muscles in the back of your throat relax too much to allow normal breathing. These muscles support structures including the back of the roof of your mouth (soft palate), the triangular piece of tissue hanging from the soft palate (uvula), the tonsils and the tongue.
When the muscles relax, your airway narrows or closes as you breathe in and breathing may be inadequate for 10 seconds or longer. This may lower the level of oxygen in your blood and cause a buildup of carbon dioxide.
Your brain senses this impaired breathing and briefly rouses you from sleep so that you can reopen your airway. This awakening is usually so brief that you don’t remember it.
You can awaken with shortness of breath that corrects itself quickly, within one or two deep breaths. You may make a snorting, choking or gasping sound.
This pattern can repeat itself five to 30 times or more each hour, all night long. These disruptions impair your ability to reach the desired deep, restful phases of sleep, and you’ll probably feel sleepy during your waking hours.
People with obstructive sleep apnea may not be aware that their sleep was interrupted. In fact, many people with this type of sleep apnea think they slept well all night.
Obstructive Sleep Apnea In Children
In children, causes of obstructive sleep apnea often include enlarged tonsils or adenoids and dental conditions such as a large overbite. Less common causes include a tumor or growth in the airway, and birth defects such as Down syndrome and Pierre-Robin syndrome. Down Syndrome causes enlargement of the tongue, adenoids and tonsils and there is decreased muscle tone in the upper airway. Pierre-Robin syndrome actually has a small lower jaw and the tongue tends to ball up and fall to the back of the throat. Although childhood obesity may cause obstructive sleep apnea, it’s much less commonly associated with the condition than adult obesity.
Risk factors
Anyone can develop obstructive sleep apnea. However, certain factors put you at increased risk, including:
Most but not all people with obstructive sleep apnea are overweight. Fat deposits around the upper airway may obstruct breathing. Medical conditions that are associated with obesity, such as hypothyroidism and polycystic ovary syndrome, also can cause obstructive sleep apnea.However, not everyone with obstructive sleep apnea is overweight and vice versa. Thin people can develop the disorder, too.Narrowed airway. You may inherit naturally narrow airways. Or your tonsils or adenoids may become enlarged, which can block your airway.
-
High blood pressure (hypertension).
Obstructive sleep apnea is relatively common in people with hypertension.
- Chronic nasal congestion. Obstructive sleep apnea occurs twice as often in those who have consistent nasal congestion at night, regardless of the cause. This may be due to narrowed airways.
Smoking.
People who smoke are more likely to have obstructive sleep apnea.
Obstructive sleep apnea may be more common in people with diabetes.
In general, men are twice as likely as premenopausal women to have obstructive sleep apnea. The frequency of obstructive sleep apnea increases in women after menopause.
- A family history of sleep apnea. If you have family members with obstructive sleep apnea, you may be at increased risk.
- Asthma. Research has found an association between asthma and the risk of obstructive sleep apnea.
Complications
Obstructive sleep apnea is considered a serious medical condition. Complications may include:
Daytime fatigue and sleepiness. The repeated awakenings associated with obstructive sleep apnea make normal, restorative sleep impossible.
People with obstructive sleep apnea often experience severe daytime drowsiness, fatigue and irritability. They may have difficulty concentrating and find themselves falling asleep at work, while watching TV or even when driving. They may also be at higher risk of work-related accidents.
Children and young people with obstructive sleep apnea may do poorly in school and commonly have attention or behavior problems.
Cardiovascular problems. Sudden drops in blood oxygen levels that occur during obstructive sleep apnea increase blood pressure and strain the cardiovascular system. Many people with obstructive sleep apnea develop high blood pressure (hypertension), which can increase the risk of heart disease.
The more severe the obstructive sleep apnea, the greater the risk of coronary artery disease, heart attack, heart failure and stroke.
Obstructive sleep apnea increases the risk of abnormal heart rhythms (arrhythmias). These abnormal rhythms can lower blood pressure. If there’s underlying heart disease, these repeated multiple episodes of arrhythmias could lead to sudden death.
Complications with medications and surgery. Obstructive sleep apnea also is a concern with certain medications and general anesthesia. These medications, such as sedatives, narcotic analgesics and general anesthetics, relax your upper airway and may worsen your obstructive sleep apnea.
If you have obstructive sleep apnea, you may experience worse breathing problems after major surgery, especially after being sedated and lying on your back. People with obstructive sleep apnea may be more prone to complications after surgery.
Before you have surgery, tell your doctor if you have obstructive sleep apnea or symptoms related to obstructive sleep apnea. If you have obstructive sleep apnea symptoms, your doctor may test you for obstructive sleep apnea prior to surgery.
Eye problems. Some research has found a connection between obstructive sleep apnea and certain eye conditions, such as glaucoma. Eye complications can usually be treated.
Sleep-deprived partners. Loud snoring can keep those around you from getting good rest and eventually disrupt your relationships. Some partners may even choose to sleep in another room. Many bed partners of people who snore are sleep deprived as well.
Diagnosis:
A sleep specialist may conduct additional evaluations to diagnose your condition, determine the severity of your condition and plan your treatment. The evaluation may involve overnight monitoring of your breathing and other body functions as you sleep.
A sleep specialist may conduct additional evaluations to diagnose your condition, determine the severity of your condition and plan your treatment. The evaluation may involve overnight monitoring of your breathing and other body functions as you sleep.
Tests to detect obstructive sleep apnea include:
Polysomnography.
During this sleep study, you’re hooked up to equipment that monitors your heart, lung and brain activity, breathing patterns, arm and leg movements, and blood oxygen levels while you sleep.
You may have a full-night study, in which you’re monitored all night, or a split-night sleep study.
In a split-night sleep study, you’ll be monitored during the first half of the night. If you’re diagnosed with obstructive sleep apnea, staff may wake you and give you continuous positive airway pressure for the second half of the night.
Polysomnography can help your doctor diagnose obstructive sleep apnea and adjust positive airway pressure therapy, if appropriate.
This sleep study can also help rule out other sleep disorders that can cause excessive daytime sleepiness but require different treatments, such as leg movements during sleep (periodic limb movements) or sudden bouts of sleep during the day (narcolepsy).
Home sleep apnea testing. Under certain circumstances, your doctor may provide you with an at-home version of polysomnography to diagnose obstructive sleep apnea. This test usually involves measurement of airflow, breathing patterns and blood oxygen levels, and possibly limb movements and snoring intensity.
Treatment
For milder cases of obstructive sleep apnea, your doctor may recommend lifestyle changes:
- Lose weight if you’re overweight.
- Exercise regularly.
- Drink alcohol moderately, if at all, and don’t drink several hours before bedtime.
- Quit smoking.
- Use a nasal decongestant or allergy medications.
- Don’t sleep on your back.
Avoid taking sedative medications such as anti-anxiety drugs or sleeping pills.
If these measures don’t improve your sleep or if your apnea is moderate to severe, then your doctor may recommend other treatments. Certain devices can help open up a blocked airway. In other cases, surgery may be necessary.
Therapies

Continuous positive airway pressure (CPAP)
An oral device or Non Invasive Device.
Positive airway pressure. If you have obstructive sleep apnea, you may benefit from positive airway pressure. In this treatment, a machine delivers air pressure through a piece that fits into your nose or is placed over your nose and mouth while you sleep.
Positive airway pressure reduces the number of respiratory events that occur as you sleep, reduces daytime sleepiness and improves your quality of life.
The most common type is called continuous positive airway pressure, or CPAP (SEE-pap). With this treatment, the pressure of the air breathed is continuous, constant and somewhat greater than that of the surrounding air, which is just enough to keep your upper airway passages open. This air pressure prevents obstructive sleep apnea and snoring.
Although CPAP is the most consistently successful and most commonly used method of treating obstructive sleep apnea, some people find the mask cumbersome, uncomfortable or loud. However, newer machines are smaller and less noisy than older machines and there are a variety of mask designs for individual comfort.
Also, with some practice, most people learn to adjust the mask to obtain a comfortable and secure fit. You may need to try different types to find a suitable mask. Several options are available, such as nasal masks, nasal pillows or face masks.
If you’re having particular difficulties tolerating pressure, some machines have special adaptive pressure functions to improve comfort. You also may benefit from using a humidifier along with your CPAP system.
CPAP may be given at a continuous (fixed) pressure or varied (autotitrating) pressure. In fixed CPAP, the pressure stays constant. In autotitrating CPAP, the levels of pressure are adjusted if the device senses increased airway resistance.
CPAP is more commonly used because it’s been well studied for obstructive sleep apnea and has been shown to effectively treat obstructive sleep apnea. However, for people who have difficulty tolerating fixed CPAP, BPAP or autotitrating CPAP may be worth a try.
Don’t stop using your positive airway pressure machine if you have problems. Check with your doctor to see what adjustments you can make to improve its comfort.
In addition, contact your doctor if you still snore despite treatment, if you begin snoring again or if your weight goes up or down by 10% or more.
Mouthpiece (oral device). Though positive airway pressure is often an effective treatment, oral appliances are an alternative for some people with mild or moderate obstructive sleep apnea. These devices may reduce your sleepiness and improve your quality of life.
These devices are designed to keep your throat open. Some devices keep your airway open by bringing your lower jaw forward, which can sometimes relieve snoring and obstructive sleep apnea. Other devices hold your tongue in a different position.
If you and your doctor decide to explore this option, you’ll need to see a dentist experienced in dental sleep medicine appliances for the fitting and follow-up therapy. A number of devices are available. Close follow-up is needed to ensure successful treatment.
Surgery or other procedures
Surgery is usually considered only if other therapies haven’t been effective or haven’t been appropriate options for you. Surgical options may include:
Surgical removal of tissue. Uvulopalatopharyngoplasty (UPPP) is a procedure in which your doctor removes tissue from the back of your mouth and top of your throat. Your tonsils and adenoids may be removed as well. UPPP usually is performed in a hospital and requires a general anesthetic.
Doctors sometimes remove tissue from the back of the throat with a laser (laser-assisted uvulopalatoplasty) or with radiofrequency energy (radiofrequency ablation) to treat snoring. These procedures don’t treat obstructive sleep apnea, but they may reduce snoring.
Upper airway stimulation. This new device is approved for use in people with moderate to severe obstructive sleep apnea who can’t tolerate CPAP or BPAP.
A small, thin impulse generator (hypoglossal nerve stimulator) is implanted under the skin in the upper chest. The device detects your breathing patterns and, when necessary, stimulates the nerve that controls movement of the tongue.
Studies have found that upper airway stimulation leads to significant improvement in obstructive sleep apnea symptoms and improvements in quality of life.
Jaw surgery (maxillomandibular advancement). In this procedure, the upper and lower parts of your jaw are moved forward from the rest of your facial bones. This enlarges the space behind the tongue and soft palate, making obstruction less likely.
Surgical opening in the neck (tracheostomy). You may need this form of surgery if other treatments have failed and you have severe, life-threatening obstructive sleep apnea.
During a tracheostomy, your surgeon makes an opening in your neck and inserts a metal or plastic tube through which you breathe. Air passes in and out of your lungs, bypassing the blocked air passage in your throat.
Implants. This minimally invasive treatment involves placement of three tiny polyester rods in the soft palate. These inserts stiffen and support the tissue of the soft palate and reduce upper airway collapse and snoring. This treatment is recommended only for people with mild obstructive sleep apnea.
Other types of surgery may help reduce snoring and sleep apnea by clearing or enlarging air passages, including:
Nasal surgery to remove polyps or straighten a crooked partition between your nostrils (deviated septum)
Surgery to remove enlarged tonsils or adenoids
Few Myths and Facts About Obstructive Sleep Apnea
Sleep Apnea Is Just Snoring
Myth. Snoring can be a symptom of the sleep disorder, but there’s a big difference between the two. People with the condition actually stop breathing up to 400 times throughout the night. These pauses last 10 to 30 seconds, and they’re usually followed by a snort when breathing starts again. This breaks your sleep cycle and can leave you tired during the day.
Sleep Apnea Is No Big Deal
Myth. All those breaks in sleep take a toll on your body and mind. When the condition goes untreated, it’s been linked to job-related injuries, car accidents, heart attacks, and strokes.
It Blocks Your Breathing
Fact. The most common type of the disorder is obstructive sleep apnea, or OSA. It happens when your tongue, tonsils, or other tissues in the back of the throat block your airway. When you try to breathe in, the air can’t get through. Central sleep apnea is less common than OSA. It means the brain doesn’t always signal the body to breathe when it should
Only Older People Get It
Myth. Doctors estimate that more than 18 million Americans have sleep apnea. It’s more common after age 40, but it can affect people of all ages. You’re more likely to have the condition if you’re overweight, a man, African-American, or Latino. The disorder also tends to run in families.
Alcohol Will Help You Sleep
Myth. A nightcap may make you drowsy, but it won’t help you get the quality rest you need. Alcohol relaxes the muscles in the back of your throat. That makes it easier for the airway to become blocked in people with sleep apnea. Sleeping pills have the same effect.
Surgery Is the Surest Way to Fix Apnea
Myth. For some people, an operation may be able to cure OSA. A good example is a child with large tonsils that block her airway. Doctors can remove the tonsils to solve the problem. Some adults can improve their symptoms with surgery to shrink or stiffen floppy tissues. But that’s not a good choice for everyone. Talk to your doctor about the pros and cons of an operation before you go that route.
CPAP Is an Effective Treatment
Fact. It stands for continuous positive airway pressure. A CPAP machine blows a steady stream of air into your airway. You can adjust the flow until it’s strong enough to keep your airway open while you sleep. It’s the most common treatment for adults with moderate to severe OSA.
Suggested Reading : Sleep Apnea