Aicardi syndrome is a rare genetic disorder that interferes with the formation of the corpus callosum, which is the structure that connects the two sides of the brain. In people with Aicardi syndrome, the corpus callosum is either partially or completely missing. The disorder occurs almost exclusively in newborn girls. Medical researchers don’t believe the disorder is passed from the parents to their child.
The exact cause of Aicardi syndrome isn’t known. However, it’s thought to be caused by a first-time mutation in the child’s genes. Since the disorder primarily affects females, researchers believe the mutation specifically occurs on the X chromosome, which is one of the two sex chromosomes. Females have two X chromosomes. Males typically have one X chromosome and one Y chromosome.
People with Aicardi syndrome often have the following:
- a partial or complete absence of the corpus callosum
- infantile spasms or seizures that begin during infancy
- chorioretinal lacunae, or lesions in the light-sensitive layer of tissue at the back of the eye
Not all people with Aicardi syndrome have these features. However, some people may display additional abnormalities in the brain, eyes, and face. The severity of symptoms varies significantly from one person to another. Some have very severe seizures and may not survive past childhood, while others have milder symptoms and may live well into adulthood.

Aicardi syndrome symptoms usually appear in babies between the ages of 2 and 5 months old. Your child may begin jerking or having infantile spasms, a type of seizure that occurs in infants. These seizures can develop into epilepsy later in life. Your child may also develop yellowish spots on their eyes. Lesions on the retina, which is the light-sensitive layer of tissue at the back of the eye, cause these spots.
Other symptoms of Aicardi syndrome include:
- a coloboma, which is a hole or gap in one of the structures of the eye
- abnormally small eyes
- an unusually small head
- hand deformities
- intellectual disabilities
- developmental delays
- difficulty eating
- diarrhea
- constipation
- gastroesophageal reflux
- spasticity, which is a condition that causes stiff and rigid muscles
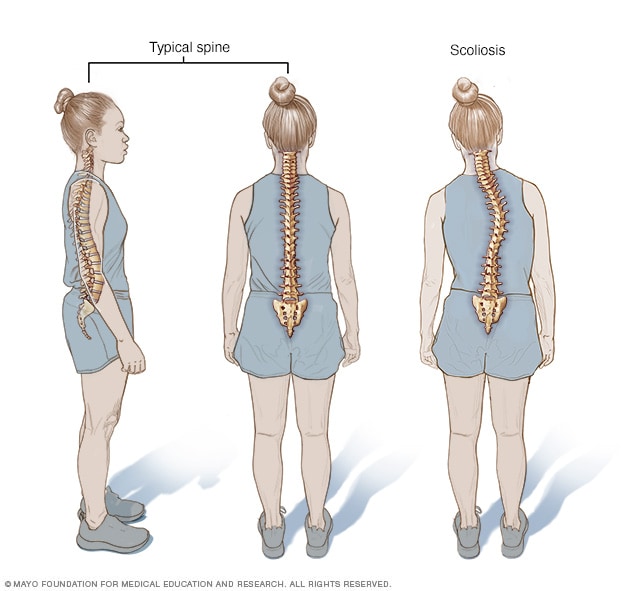
Additional symptoms of Aicardi syndrome include rib and spine abnormalities, such as scoliosis. Children with this disorder may also have unusual facial features, such as a flatter nose, larger ears, or a smaller space between the upper lip and nose. Since Aicardi syndrome can result in poorly developed eyes, children may experience impaired vision or blindness.
Researchers have also found that the brains of children with Aicardi syndrome may have fewer folds and grooves than a normal brain. Fluid-filled cysts may also be present in the brain.
Aicardi syndrome most often appears in females as well as in boys with Klinefelter’s syndrome, a condition in which a male has an extra X chromosome. For these reasons, researchers believe the disorder is caused by a defect on the X chromosome.
People normally have 46 chromosomes in each cell. Two of the 46 chromosomes are sex chromosomes, known as X and Y. They help determine whether someone will develop male or female sex characteristics. Females have two X chromosomes, while males usually have one X chromosome and one Y chromosome.
During the normal development of an embryo, there should only be one active X chromosome in each cell. This means that one of the two X chromosomes in a female embryo must randomly deactivate during cell formation. In the case of Aicardi syndrome, researchers think that the deactivation of the X chromosomes fails to alternate randomly. As a result, one X chromosome is active in more than half of the body’s cell formations. This is called “skewed X-inactivation.”
Researchers have yet to determine the exact gene that causes skewed X-inactivation, so the cause of the disorder is still not known. This lack of information also makes it difficult to determine the risk factors for Aicardi syndrome.
Doctors can usually diagnose Aicardi syndrome based on the symptoms. However, since each child may present different symptoms, additional tests may be needed. Some tests that are used to help doctors make a diagnosis include:
- eye exams
- an electroencephalogram (EEG), which evaluates the electrical activity of the brain and detects seizure activity
- an MRI or CT scan, which provides detailed anatomical images of the head and brain
There’s no cure for Aicardi syndrome at this time. However, some symptoms can be managed with treatment. The most common method of treatment involves controlling the seizures and spasms brought on by the disorder. There are also programs available to help both children and their parents cope with the intellectual disabilities and developmental delays that usually accompany Aicardi syndrome. Your child’s doctor will likely refer you to a pediatric neurologist for further evaluation. A pediatric neurologist is a doctor who specializes in treating nervous system disorders in children. They can help your child with long-term management of Aicardi syndrome. Doctors in these other fields may also be may also be consulted based on the symptoms and severity of the syndrome:
- neurosurgery
- ophthalmology
- orthopedics
- gastroenterology
- physical therapy
- speech therapy
- occupational therapy