Aortic valve stenosis occurs when the aortic valve narrows and doesn’t open as it should. This limits the amount of blood pumped from your heart into, and then out of, the aorta. This is the main artery of the body. The aortic valve is a key valve in the body’s blood circulation system.
Aortic valve stenosis generally produces symptoms only once it progresses. You may not have symptoms in the beginning.
You may experience symptoms of severe aortic valve stenosis once the condition has progressed to the symptomatic stage. Symptoms of severe aortic valve stenosis include:
- chest pain as the heart strains to pump enough blood through the compromised valve
- feeling tired after exertion, as when you exercise or move
- feeling short of breath, especially after exertion
- heart palpitations, or abnormal heartbeats
- a heart murmur, which is an abnormal swooshing sound produced by the heart as it beats
Infants and children may have different symptoms from adults, or they may not appear to display any symptoms at all. If they do display symptoms, these might include:
- inability to put on weight
- not eating well
- becoming easily fatigued
In severe cases, an infant may have major breathing difficulties that develop within weeks of birth. Mild cases have the potential to worsen as the child gets older.
Causes:
Genetics and certain health conditions may prevent the aortic valve from completing its proper functions. The aortic valve opens and closes every time your heart beats. This continuous action occurs every second of your life.
Genetics
Aortic valve stenosis may be present at birth. When it is, the flaps, or “leaflets,” of the aortic valve are irregularly formed. These leaflets make up the opening of the aortic valve. When functioning properly, they fit together tightly when closed. Children born with aortic valve stenosis usually have one of the following irregularities in their aortic valve leaflets:
- All three leaflets aren’t present.
- The leaflets don’t separate properly.
- The leaflets are too thick to completely open or close.
Rheumatic fever
Rheumatic fever is one of the most common causes of heart valve problems. Rheumatic fever may affect many parts of the body, including the:
- brain
- joints
- heart
- skin
Rheumatic fever can occur in adults and children who have, or have had, strep throat. Strep throat is a contagious condition caused by Streptococcus bacteria.
Calcification of the valves
Aortic valve stenosis most often occurs in older adults. Age-related aortic valve stenosis is the most common form of the condition, according to the American Heart Association. It’s caused by calcification or scarring of the aortic valve. It usually begins sometime after the age of 60, but people may not begin to experience symptoms until age 70 or 80.
Calcium is an important mineral needed for strong bones. However, the mineral may lead to problems in your heart if it deposits in the aortic valve. Calcium deposits usually affect the leaflets of the aortic valve. They can also prevent the aortic valve from properly opening and closing. These deposits often increase in the aortic valve as we age due to scarring and calcium buildup.
Improperly functioning aortic valve leaflets may also allow blood to leak back into the left ventricle after it enters the aorta. This is called valvular insufficiency, or regurgitation.
Gender
Men have a higher risk of aortic valve stenosis than women. The condition occurs most often in men between the ages of 30 and 60.
Genetics
Children born with either malformed valve leaflets or fewer than three leaflets will have problems with normal blood flow through the aorta.
Disease
Rheumatic fever can produce significant problems with the valve leaflets. Scar tissue from the disease can make the leaflets hard or even fused. Rheumatic fever damages:
- heart tissue
- valves
- coronary arteries
There are no specific medications to fix aortic valve stenosis. This is because the condition is irreversible once it occurs. Instead, your doctor can prescribe medication to treat the problems caused by the condition, or for the health issues that produced the condition in the first place. Surgery may be able to repair or replace the valve.
Medications
Although medication can’t cure aortic valve stenosis, your doctor may prescribe drugs to manage symptoms or reduce the burden on your heart. Some medications include:
- Antibiotics. Rheumatic fever requires antibiotics to keep any infection from advancing and causing heart damage.
- Blood pressure medications. Beta-blockers or calcium channel blockers can help lower your blood pressure.
- Blood thinners. Blood thinners such as Coumadin may be necessary.
- Anti-arrhythmics. Medications to manage your heart’s rhythm, called anti-arrhythmics, are sometimes prescribed.
Surgery options include:
Aortic valve repair
-
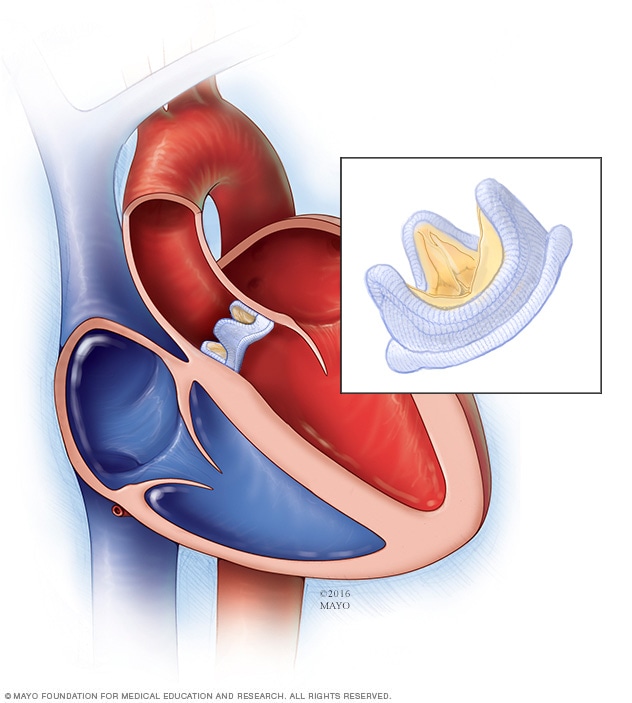
Biological valve replacement
Surgeons rarely repair an aortic valve to treat aortic valve stenosis, and generally aortic valve stenosis requires aortic valve replacement. To repair an aortic valve, surgeons may separate valve flaps (cusps) that have fused.
Balloon valvuloplasty
Doctors may conduct a procedure using a long, thin tube (catheter) to repair a valve with a narrowed opening (aortic valve stenosis). In this procedure, called balloon valvuloplasty, a doctor inserts a catheter with a balloon on the tip into an artery in your arm or groin and guides it to the aortic valve. The doctor performing the procedure then inflates the balloon, which expands the opening of the valve. The balloon is then deflated, and the catheter and balloon are removed.
The procedure can treat aortic valve stenosis in infants and children. However, the valve tends to narrow again in adults who’ve had the procedure, so it’s usually only performed in adults who are too ill for surgery or who are waiting for a valve replacement, as they typically need additional procedures to treat the narrowed valve over time.
Aortic valve replacement
-
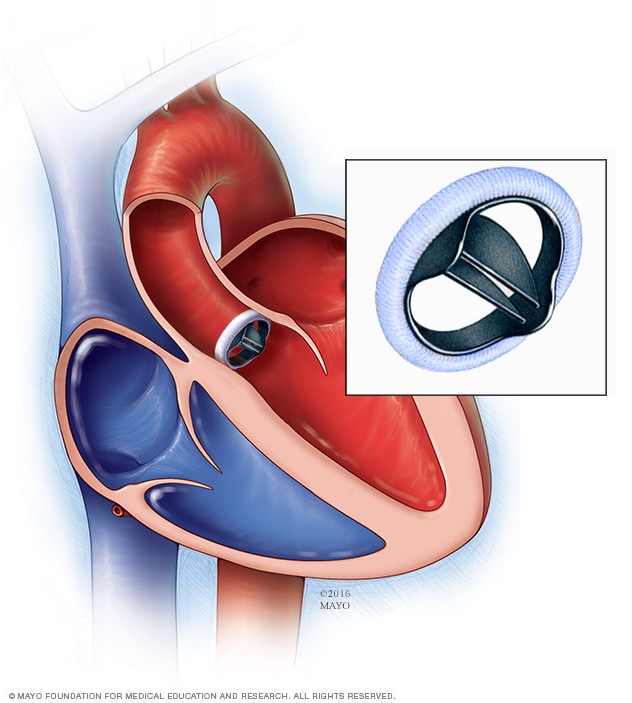
Mechanical valve replacement
Aortic valve replacement is often needed to treat aortic valve stenosis. In aortic valve replacement, your surgeon removes the damaged valve and replaces it with a mechanical valve or a valve made from cow, pig or human heart tissue (biological tissue valve).
Biological tissue valves degenerate over time and may eventually need to be replaced. People with mechanical valves will need to take blood-thinning medications for life to prevent blood clots. Your doctor will discuss with you the benefits and risks of each type of valve and discuss which valve may be appropriate for you.
-
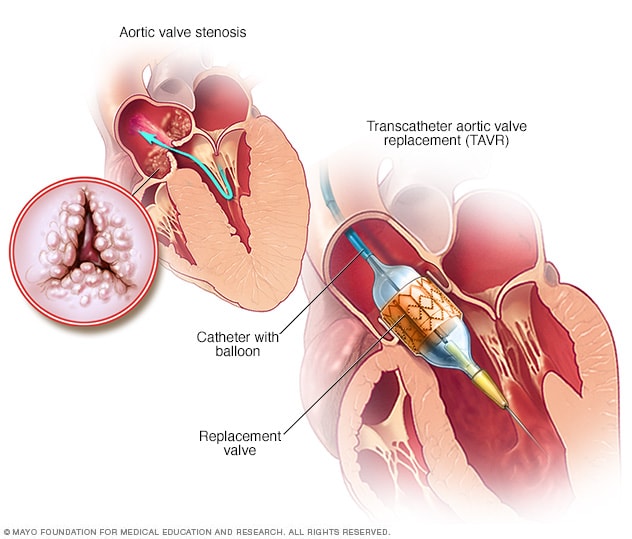
Transcatheter aortic valve replacement (TAVR)
Doctors may perform a less invasive procedure called transcatheter aortic valve replacement (TAVR) to replace a narrowed aortic valve. TAVR may be an option for people who are considered to be at intermediate or high risk of complications from surgical aortic valve replacement.
In TAVR, doctors insert a catheter in your leg or chest and guide it to your heart. A replacement valve is then inserted through the catheter and guided to your heart. A balloon may expand the valve, or some valves can self-expand. When the valve is implanted, doctors remove the catheter from your blood vessel.
Doctors may also conduct a catheter procedure to insert a replacement valve into a failing biological tissue valve that is no longer working properly. Other catheter procedures to repair or replace aortic valves continue to be researched.
Lifestyle and home remedies
You’ll have regular follow-up appointments with your doctor to monitor your condition. You’ll need to continue taking all your medications as prescribed.
Your doctor may suggest you incorporate several heart-healthy lifestyle changes into your life, including:
- Eating a heart-healthy diet. Eat a variety of fruits and vegetables, low-fat or fat-free dairy products, poultry, fish, and whole grains. Avoid saturated and trans fat, and excess salt and sugar.
- Maintaining a healthy weight. Aim to keep a healthy weight. If you’re overweight or obese, your doctor may recommend that you lose weight.
- Getting regular physical activity. Aim to include about 30 minutes of physical activity, such as brisk walks, into your daily fitness routine.
- Managing stress. Find ways to help manage your stress, such as through relaxation activities, meditation, physical activity, and spending time with family and friends.
- Avoiding tobacco. If you smoke, quit. Ask your doctor about resources to help you quit smoking. Joining a support group may be helpful.
For women with aortic valve stenosis, it’s important to talk with your doctor before you become pregnant. Your doctor can discuss with you which medications you can safely take, and whether you may need a procedure to treat your valve condition prior to pregnancy.
You’ll likely require close monitoring by your doctor during pregnancy. Doctors may recommend that women with severe valve stenosis avoid pregnancy to avoid the risk of complications.
Long-term outlook
Your health may improve dramatically once you receive treatment. Surgical treatments for aortic valve stenosis have high rates of success. Your outlook depends on a combination of factors:
- how long you’ve lived with the condition
- the extent of damage to your heart
- any complications that may arise from your condition
Sometimes, aortic valve stenosis isn’t a congenital defect, meaning you weren’t born with the condition. If this is the case, there are healthy lifestyle steps you can take to ease the burden on your heart:
- Eat a healthy diet low in saturated fat.
- Exercise regularly.
- Maintain a healthy weight.
- Abstain from smoking.
- Report any abnormal health issues to your doctor.
- Visit your doctor for any severe sore throat to prevent rheumatic fever.
- Practice good dental hygiene, as dental infections can travel through the bloodstream and damage the heart valves and muscles.