Hair transplant surgery is surgery that is performed to restore hair to areas of the scalp that are bald or that have thinning hair. There are multiple types of hair replacement surgery. Most commonly, these involve hair transplantation, but flap surgery, tissue expansion of the scalp and scalp reduction surgery, are also methods used for hair replacement. Each of these types of surgeries can be used alone, or in combination, to provide the patient with the best possible outcome for hair replacement.
Hair transplantation involves removing small pieces of hair-bearing scalp from a donor site and using them as grafts to be relocated to a bald or thinning area of the scalp.
Flaps surgeries involve moving hair bearing scalp tissue into bald areas of the scalp.
Tissue expansion allows the hair bearing scalp to be expanded to help cover areas of the scalp that have no hair.
Scalp reduction surgery involves surgically removing bald areas of the scalp and advancing, or bringing together, the hair bearing areas of the scalp.
If you and your surgeon have determined that hair transplant surgery is the best option for you, you can feel comfortable knowing that board-certified plastic surgeons have been successfully performing these types of procedures for more than thirty years.
The truth about hair loss
Baldness is often blamed on poor circulation to the scalp, vitamin deficiencies, dandruff and even excessive hat wearing. All of these theories have been disproved. It’s also untrue that hair loss can be determined by looking at your maternal grandfather, or that 40-year-old men who haven’t lost their hair will never lose it.
Hair loss is primarily caused by a combination of:
- Aging
- A change in hormones
- A family history of baldness
Hair transplantation steps:
Hair transplantation involves removing small punch grafts from the hair bearing scalp or a larger piece of this scalp from a donor area and cutting this into smaller pieces to use as grafts. These grafts are then relocating to a bald or thinning area of the scalp. The grafts created in this manner differ in size and shape. Round-shaped punch grafts usually contain about 10-15 hairs. The much smaller mini-graft contains about two to four hairs; and the micro-graft, one to two hairs. Slit grafts, which are inserted into slits created in the scalp, contain about four to 10 hairs each; strip grafts are long and thin and contain 30-40 hairs.
Generally, several surgical sessions may be needed to achieve satisfactory fullness, and a healing interval of several months is usually recommended between each session. It may take up to two years before you see the final result with a full transplant series. The amount of coverage you’ll need is partly dependent upon the color and texture of your hair. Coarse, gray or light-colored hair affords better coverage than fine, dark-colored hair. The number of large plugs transplanted in the first session varies with each individual, but the average is about 50. For mini-grafts or micro-grafts, the number can be up to 700 per session.
Just before surgery, the “donor area” will be trimmed short so that the grafts can be easily accessed and removed. For punch grafts, your doctor may use a special tube-like instrument made of sharp carbon steel that punches the round graft out of the donor site so it can be replaced in the area to be covered—generally the frontal hairline. For other types of grafts, your doctor will use a scalpel to remove small sections of hair-bearing scalp, which will be divided into tiny sections and transplanted into tiny holes or slits within the scalp. When grafts are taken, your doctor may periodically inject small amounts of saline solution into the scalp to maintain proper skin strength. The donor site holes may be closed with stitches—for punch grafts, a single stitch may close each punch site; for other types of grafts, a small, straight-line scar will result. The stitches are usually concealed with the surrounding hair.
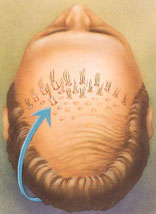
To maintain healthy circulation in the scalp, the grafts are placed about one-eighth of an inch apart. In later sessions, the spaces between the plugs will be filled in with additional grafts. Your doctor will take great care in removing and placement of grafts to ensure that the transplanted hair will grow in a natural direction and that hair growth at the donor site is not adversely affected.
After the grafting session is complete, the scalp will be cleansed and covered with gauze. You may have to wear a pressure bandage for a day or two. Some doctors allow their patients to recover bandage-free.
Tissue Expansion
Another technique used in the treatment of baldness is called tissue expansion. Plastic surgeons are the leaders in tissue expansion, a procedure commonly used in reconstructive surgery to repair burn wounds and injuries with significant skin loss. Its application in hair transplant surgery has yielded dramatic results-significant coverage in a relatively short amount of time.
In this technique, a balloon-like device called a tissue expander is inserted beneath hair-bearing scalp that lies next to a bald area. The device is gradually inflated with salt water over a period of weeks, causing the skin to expand and grow new skin cells. This causes a bulge beneath the hair-bearing scalp, especially after several weeks.
When the skin beneath the hair has stretched enough-usually about two months after the first operation-another procedure is performed to bring the expanded skin over to cover the adjacent bald area. For more information about tissue expansion, ask your plastic surgeon for the American Society of Plastic Surgeons, Inc. brochure entitled, Tissue Expansion: Creating New Skin from Old.
Flap Surgery
Flap surgery on the scalp has been performed successfully for more than 20 years. This procedure is capable of quickly covering large areas of baldness and is customized for each individual patient. The size of the flap and its placement are largely dependent upon the patient’s goals and needs. One flap can do the work of 350 or more punch grafts.
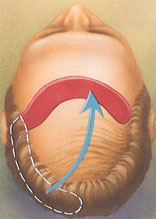
A section of bald scalp is cut out and a flap of hair-bearing skin is lifted off the surface while still attached at one end. The hair-bearing flap is brought into its new position and sewn into place, while remaining “tethered” to its original blood supply. As you heal, you’ll notice that the scar is camouflaged—or at least obscured—by relocated hair, which grows to the very edge of the incision.
In recent years, plastic surgeons have made significant advances in flap techniques, combining flap surgery and scalp reduction for better coverage of the crown; or with tissue expansion, to provide better frontal coverage and a more natural hairline.
Scalp Reduction
This technique is sometimes referred to as advancement flap surgery because sections of hair-bearing scalp are pulled forward or “advanced” to fill in a bald crown.
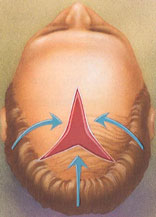
Scalp reduction is for coverage of bald areas at the top and back of the head. It’s not beneficial for coverage of the frontal hairline. After the scalp is injected with a local anesthetic, a segment of bald scalp is removed. The pattern of the section of removed scalp varies widely, depending on the patient’s goals. If a large amount of coverage is needed, doctors commonly remove a segment of scalp in an inverted Y-shape. Excisions may also be shaped like a U, a pointed oval or some other figure.
The skin surrounding the cut-out area is loosened and pulled, so that the sections of hair-bearing scalp can be brought together and closed with stitches. It’s likely that you’ll feel a strong tugging at this point, and occasional pain.
Procedure Steps
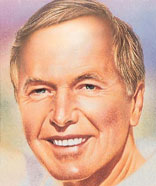
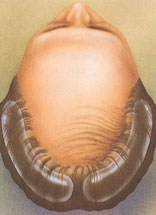
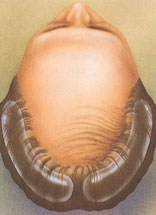
Before: Hair transplant candidates should have some noticeable hair loss with healthy hair growth at the back and sides of the head to serve as donor areas.
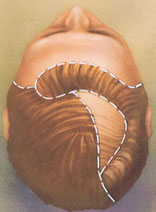
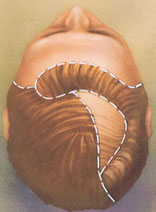
Step 1: A tube-like instrument punches round grafts from the donor site to be placed in the area where hair replacement is desired.
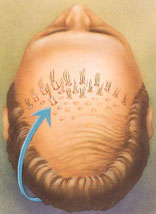
Step 2: A tube-like instrument punches round grafts from the donor site to be placed in the area where hair replacement is desired.
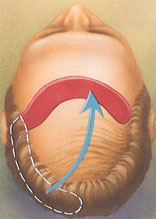
Step 3: When the skin beneath the hair has stretched enough, it is surgically placed over the bald area.
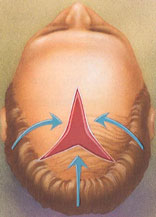
Step 4: During flap surgery, a section of bald scalp is cut out and a flap of hair-bearing skin is sewn into its place.
Step 5: The patterns used in scalp reduction vary widely, yet all meet the goal of bringing hair and scalp together to cover bald areas.
After: The results of hair transplant surgery can enhance your appearance and self-confidence.