Diabetic neuropathy is a serious and common complication of type 1 and type 2 diabetes. It’s a type of nerve damage caused by uncontrolled high blood sugar levels. You may not initially have any symptoms. The condition usually develops slowly, sometimes over the course of several decades.
Types of diabetic neuropathy include the following:
- Peripheral neuropathy
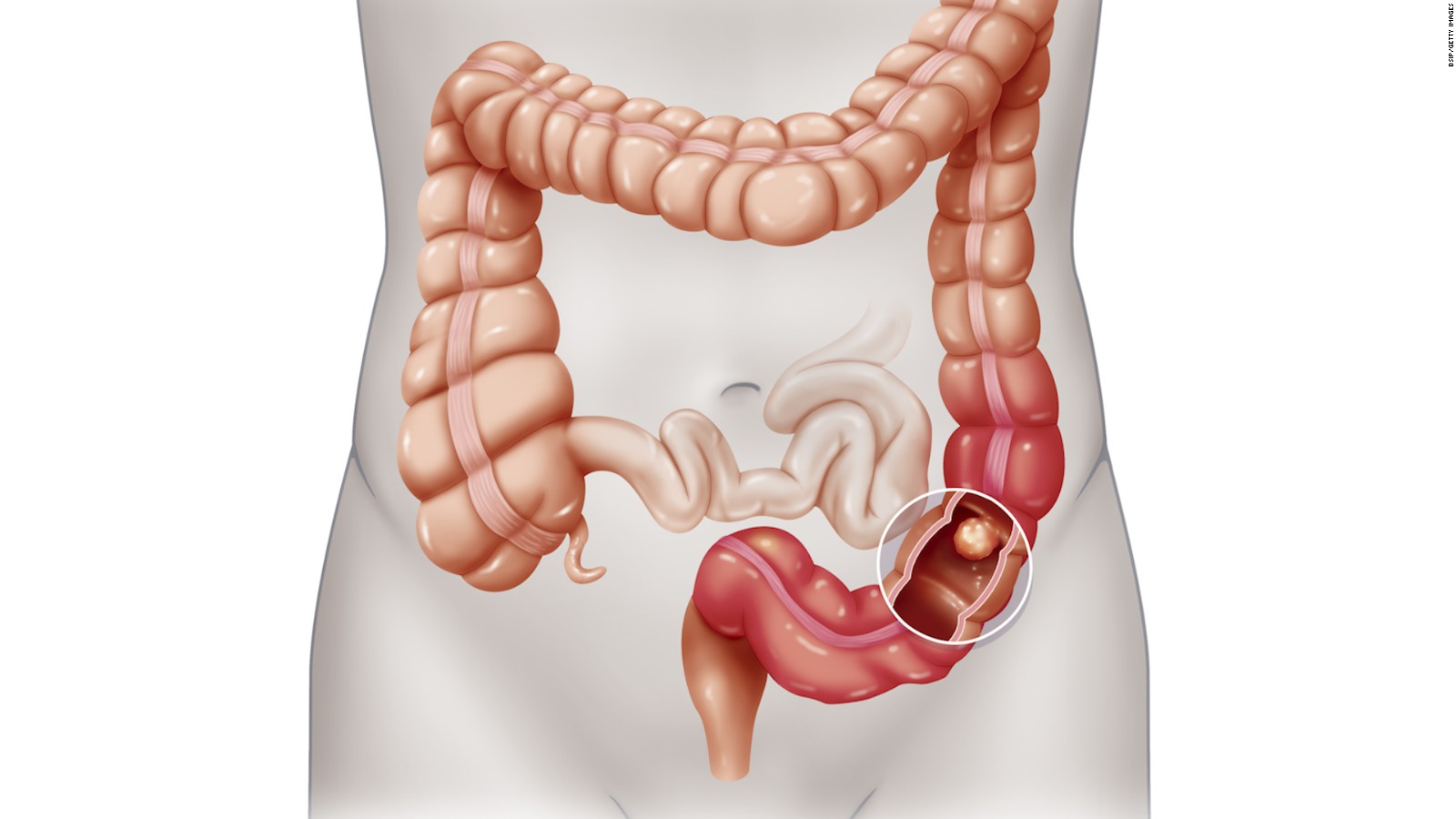
- Autonomic neuropathy
- Focal neuropathies
- Proximal neuropathy
If you have diabetes, your chance of developing nerve damage caused by diabetes increases the older you get and the longer you have diabetes. Managing your diabetes is an important part of preventing health problems such as diabetic neuropathy.
Your symptoms depend on which type of diabetic neuropathy you have. In peripheral neuropathy, some people may have a loss of sensation in their feet, while others may have burning or shooting pain in their lower legs. Most nerve damage develops over many years, and some people may not notice symptoms of mild nerve damage for a long time. In some people, severe pain begins suddenly.
Foot care is very important for all people with diabetes, and it’s even more important if you have peripheral neuropathy. Check your feet for problems every day, and take good care of your feet. See your doctor for a neurological exam and a foot exam at least once a year and more often if you have foot problems.
to know more details:- send in your queries to query@gtsmeditour.com or WhatsApp your latest medical reports to +91-9880149003.