
Middle East Respiratory Syndrome (MERS) is viral respiratory illness that is new to humans. It was first reported in Saudi Arabia in 2012 and has since spread to several other countries, including the United States.Middle East Respiratory Syndrome (MERS) is an illness caused by a virus (more specifically, a coronavirus) called Middle East Respiratory Syndrome Coronavirus (MERS-CoV). Most MERS patients developed severe respiratory illness with symptoms of fever, cough and shortness of breath. About 3 or 4 out of every 10 patients reported with MERS have died.
Symptoms:
Most people confirmed to have MERS-CoV infection have had severe respiratory illness with symptoms of:
- fever
- cough
- shortness of breath
- Some people also had diarrhea and nausea/vomiting.
- For many people with MERS, more severe complications followed, such as pneumonia and kidney failure.
Most of the people who died had a pre-existing medical condition that weakened their immune system, or an underlying medical condition that hadn’t yet been discovered. Medical conditions sometimes weaken people’s immune systems and make them more likely to get sick or have severe illness.
Pre-existing conditions among people who got MERS have included
diabetes
cancer
chronic lung disease
chronic heart disease
chronic kidney disease
Some infected people had mild symptoms (such as cold-like symptoms) or no symptoms at all.
The symptoms of MERS start to appear about 5 or 6 days after a person is exposed, but can range from 2 to 14 days.
Transmission
MERS-CoV, like other coronaviruses, likely spreads from an infected person’s respiratory secretions, such as through coughing. However, we don’t fully understand the precise ways that it spreads.
MERS-CoV has spread from ill people to others through close contact, such as caring for or living with an infected person. Infected people have spread MERS-CoV to others in healthcare settings, such as hospitals. Researchers studying MERS have not seen any ongoing spreading of MERS-CoV in the community.
All reported cases have been linked to countries in and near the Arabian Peninsula. Most infected people either lived in the Arabian Peninsula or recently traveled from the Arabian Peninsula before they became ill. A few people have gotten MERS after having close contact with an infected person who had recently traveled from the Arabian Peninsula. The largest known outbreak of MERS outside the Arabian Peninsula occurred in the Republic of Korea in 2015 and was associated with a traveler returning from the Arabian Peninsula.
Diagnosis:
Real-time reverse transcriptase-polymerase chain reaction (RT-PCR) testing of upper and lower respiratory secretions and serum
MERS should be suspected in patients who have an unexplained acute febrile lower respiratory infection and who have had either of the following within 14 days of symptom onset:
Travel to or residence in an area where MERS has recently been reported or where transmission could have occurred
Contact with a health care facility where MERS has been transmitted
Close contact with a patient who was ill with suspected MERS
MERS should also be suspected in patients who have had close contact with a patient with suspected MERS and who have a fever whether they have respiratory symptoms or not.
Testing should include real-time RT-PCR testing of upper and lower respiratory secretions, ideally taken from different sites and at different times. Serum should be obtained from patients and from all, even asymptomatic close contacts, including health care workers (to help identify mild or asymptomatic MERS). Serum is obtained immediately after MERS is suspected or after contacts are exposed (acute serum) and 3 to 4 weeks later (convalescent serum). Testing is done at state health departments.
Treatment:
Treatment of MERS is supportive. To help prevent spread from suspected cases, health care practitioners should use standard, contact, and airborne precautions.
There is no vaccine.
Prevention:
There is currently no vaccine to protect people against MERS. But scientists are working to develop one.
We can help reduce the risk of getting respiratory illnesses:
- Wash your hands often with soap and water for at least 20 seconds, and help young children do the same. If soap and water are not available, use an alcohol-based hand sanitizer.
- Cover your nose and mouth with a tissue when you cough or sneeze, then throw the tissue in the trash.
- Avoid touching your eyes, nose, and mouth with unwashed hands.
- Avoid personal contact, such as kissing, or sharing cups or eating utensils, with sick people.
- Clean and disinfect frequently touched surfaces and objects, such as doorknobs.
People Who May Be at Increased Risk for MERS:
- Recent Travelers from the Arabian Peninsula
If you develop a fever and symptoms of respiratory illness, such as cough or shortness of breath, within 14 days after traveling from countries in or near the Arabian Peninsula, you should call ahead to a healthcare provider and mention your recent travel.
- Close Contacts of an Ill Traveler from the Arabian Peninsula
If you have had close contact with someone within 14 days after they traveled from a country in or near the Arabian Peninsula, and the traveler has/had fever and symptoms of respiratory illness, such as cough or shortness of breath, you should monitor your health for 14 days, starting from the day you were last exposed to the ill person.
- Healthcare Personnel Not Using Recommended Infection-Control Precautions
Healthcare personnel who had close contact*** with a confirmed case of MERS while the case was ill, if not using recommended infection control precautions (e.g., appropriate use of personal protective equipment), are at increased risk of developing MERS-CoV infection. These individuals should be evaluated and monitored by a healthcare professional with a higher index of suspicion.
- Close Contacts of a Confirmed Case of MERS
f you have had close contact with someone who has a confirmed MERS-CoV infection, you should contact a healthcare provider for an evaluation. Your healthcare provider may request laboratory testing and outline additional recommendations, depending on the findings of your evaluation and whether you have symptoms.
- People with Exposure to Camels
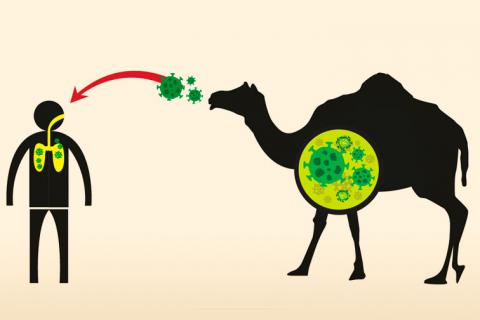
Direct contact with camels is a risk factor for human infection with MERS-CoV.
The World Health Organization considers certain groups to be at high risk for severe MERS. These groups include people with diabetes, kidney failure, or chronic lung disease, and people who have weakened immune systems. The World Health Organization recommends that these groups take additional precautions:
- Avoid contact with camels
- Do not drink raw camel milk or raw camel urine
- Do not eat undercooked meat, particularly camel meat
We’re sure, you now have a fair idea of what MERS-CoV is all about and the way it could impact your life. Please seek immediate medical attention at the nearest healthcare centre if you find the MERS-CoV. symptoms, don’t ignore the symptoms as there is no medicine available at present.
suggested reading COVID -19

Post a comment