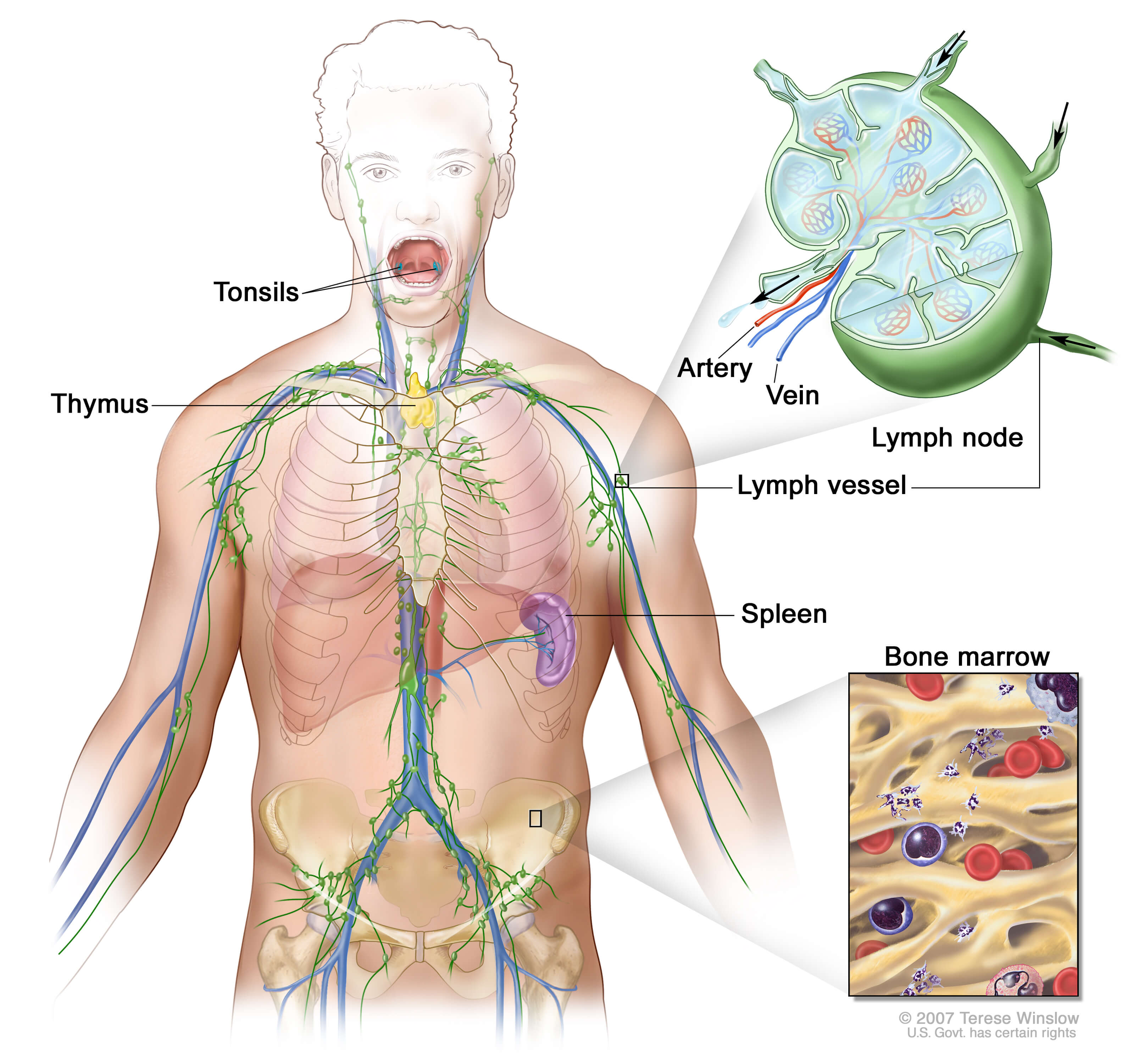
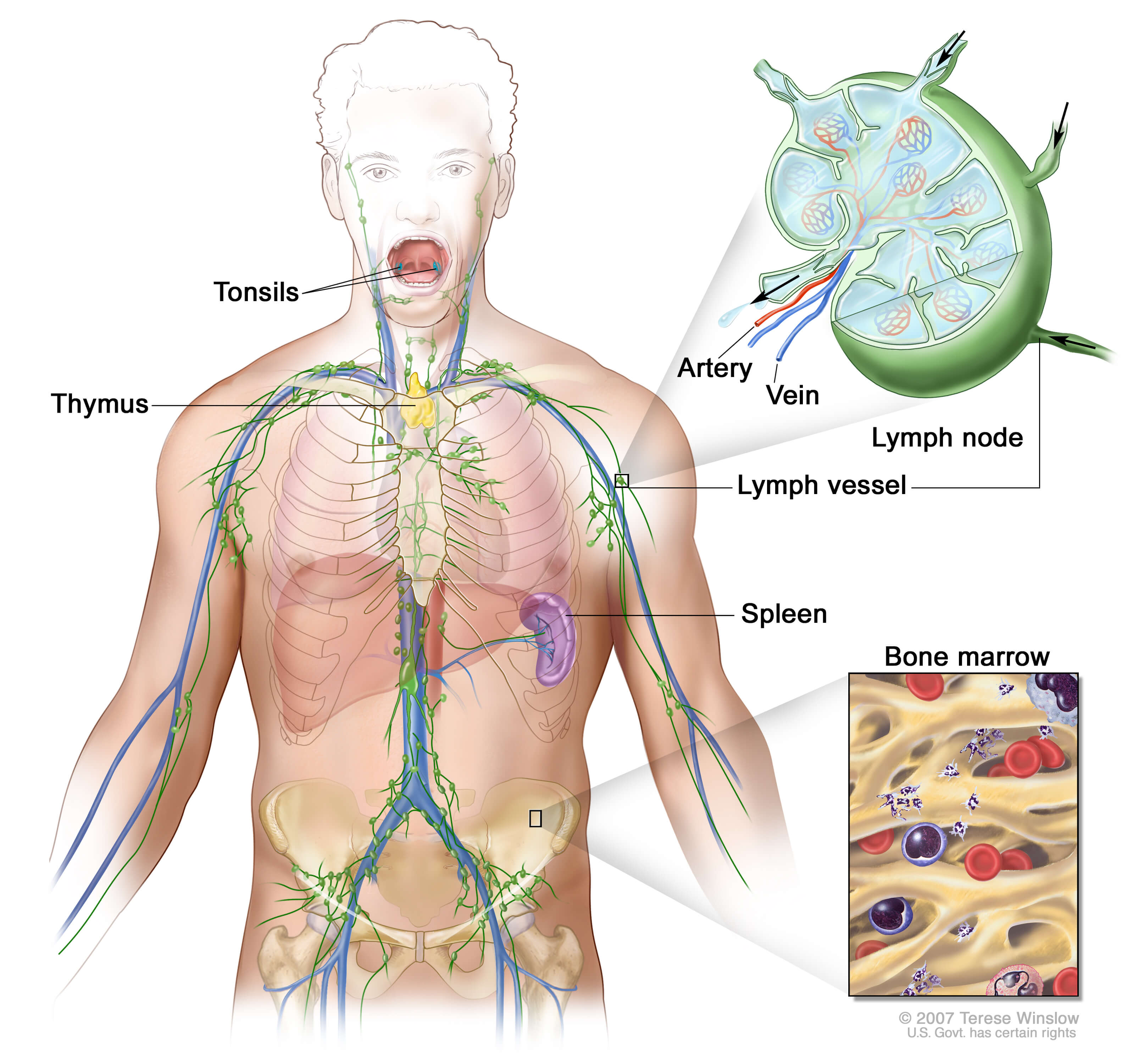
Central nervous system lymphoma is a rare non-Hodgkin lymphoma in which malignant (cancer) cells from lymph tissue form in the brain and/or spinal cord (primary CNS) or spread from other parts of the body to the brain and/or spinal cord (secondary CNS). Because the eye is so close to the brain, primary CNS lymphoma can also start in the eye (called ocular lymphoma). The cancer can also involve the spinal fluid that bathes the spinal cord and brain. This is called leptomeningeal lymphoma.
Both primary and secondary CNS lymphomas are rare diseases. The cancer is a form of extranodal, high-grade non-Hodgkin B-cell lymphoma. Most forms of CNS lymphoma (about 90 percent) are diffuse large B-cell lymphomas; the remaining ten percent are poorly characterized low-grade lymphomas, Burkitt lymphomas and T-cell lymphomas.
Central nervous system lymphoma is more common in men than women. The median age of diagnosis is 55; the median age of AIDS-infected patients with primary CNS lymphoma is 35.
Causes and Risk Factors
Although the exact causes of CNS lymphoma are not known, there are several factors that may increase a person’s risk for developing the disease, such as having a compromised immune system due to acquired immunodeficiency syndrome (AIDS), other disorders of the immune system, or chronic immunosuppression (a reduced function of the immune system) as a result of organ transplantation.
Symptoms
The symptoms of CNS lymphoma depend on the location of the tumor. Patients may experience nausea and vomiting, leg and arm weakness, seizures, headaches, changes in mental alertness or confusion, facial weakness, double vision and hearing loss and/or swallowing difficulties. Patients with ocular lymphoma may notice blurry vision and patients with lymphoma involving their spinal cord or spinal fluid may experience back pain, leg weakness or incontinence.
Diagnosis
Tests that examine the eyes, brain and spinal cord are used to find and diagnose CNS lymphoma. These tests may include
- Physical exam and history
- Neurological exam to check mental status, coordination, ability to walk normally and how well the muscles, senses and reflexes work
- Slit-lamp eye exam – This test uses a special microscope with a bright, narrow slit of light to check the outside and inside of the eye.
- Vitrectomy – A surgical procedure in which some of the vitreous humor (the gel-like fluid inside the eyeball) is removed and examined under a microscope to check for cancer cells.
- Chest x-ray and CT scans of the chest and abdomen
- MRI scans of the brain and spinal cord
- Blood and urine tests
- Lumbar puncture (or spinal tap)
- Stereotactic biopsy, in which a computer and a three-dimensional scanning device are used to find a tumor and guide the removal of tissue for examination under a microscope to look for cancer cells.
Staging
After CNS lymphoma is diagnosed, a series of tests may be done to determine whether the cancer has spread. The information is then used to stage the disease and plan treatment. At this time, patients may also want to schedule a consultation with an ophthalmologist (eye doctor).
Some tests used to stage CNS lymphoma include:
- CT scan
- PET scan
- Bone marrow aspiration and biopsy

- Slit-lamp eye exam
- Vitrectomy
- Testicular examination in men
Prognostic Factors
There are certain factors that affect prognosis (the chance of recovery) and treatment options for CNS lymphoma. These include
- The patient’s age and overall health
- Performance status
- Lactate dehydrogenase level
- Unusually higher or lower level of certain substances in the blood and cerebrospinal fluid
- Location of the tumor in the central nervous system
- Whether the patient has AIDS
Treatment
There is no standard treatment for CNS lymphoma. Your doctor will discuss the best treatment option for you. As CNS lymphoma only affects a small number of people, it is important to be treated by a hematologist/oncologist who is knowledgeable about non-Hodgkin lymphoma. It is important to consider getting a second opinion with a NHL expert to make sure you are aware of all treatment options.
Possible treatment options are listed below. Methotrexate-based combinations have been the most successful for CNS lymphoma patients. These are usually given at high doses and require that the patient be hospitalized while giving the chemotherapy. For patients over age 60 years, radiation treatment can be extremely neurotoxic and it is important to speak to your doctor before receiving this treatment. Patients who have relapsed or refractory CNS lymphoma, cytarabine and topotecan may also be an option. Talk to your doctor about the best care for you.
Treatment options for CNS lymphoma not related to AIDS include:
- Chemotherapy
- Chemotherapy followed by radiation therapy
- Steroid therapy
- Whole brain radiation therapy
- A clinical trial of high-dose chemotherapy with stem cell transplant
Treatment options for AIDs-related CNS lymphoma include:
- Steroids with or without radiation
- Radiation
- Chemotherapy followed by radiation therapy
Treatment for recurrent (the cancer comes back) CNS lymphoma includes:
- Chemotherapy or radiation (if not received as first-line treatment)
- Chemotherapy and radiation
- A clinical trial
For some patients, taking part in a clinical trial may be the best treatment choice. There are also several clinical trials available nationally that are examining the role of radiation and the role of bone marrow transplantation for the treatment of primary CNS lymphoma. Your doctor can discuss if these clinical trials are appropriate or available for you. For information about clinical trials for CNS lymphoma, please call our Information Specialists or click here for an online clinical-trial search service supported by LLS that offers patients and caregivers immediate access to listings of blood cancer clinical trials.
Treatment Outcomes
Treatment of CNS lymphoma is most effective when the tumor has not spread outside the cerebrum (the largest part of the brain) and the patient is under age 60, able to maintain daily functions and does not have AIDS or other diseases that weaken the immune system.