Systemic sclerosis (SSc) is a multisystem autoimmune disease in which there is increased fibroblast activity resulting in abnormal growth of connective tissue. This causes vascular damage and fibrosis. Fibrosis occurs in skin, the gastrointestinal (GI) tract and other internal organs.
The name scleroderma is derived from the Greek for ‘hard skin’ and emphasises the dermatological component of the disease. It was described by Hippocrates. There is a localised form of scleroderma, also known as morphoea
General features
- Fatigue.
- Weight loss.
Skin features
- Signs in the hand:
- Swelling (non-pitting oedema) of fingers and toes – a common early sign; digits may look sausage-like; hand movement may be limited.
- Skin becomes hard and thickened – this may limit joint movement or cause joint contractures; in the fingers, this is known as sclerodactyly.
- Swelling and sclerosis reduce hand movements, so patients may be unable to make a fist, or to place the palmar surfaces together – the ‘prayer sign’.
- Fingertips may have pitting, ulcers or loss of bulk from finger pads.
- Raynaud’s phenomenon. This is the most common symptom and is present at some point in 90% of cases. Raynaud’s phenomenon with puffy fingers is thought to be a cardinal sign of likely SSc.
- Calcinosis – nodules or lumps of chalky material which may break through the skin.
- Face and mouth:
- Tightening of facial skin.
- Tight lips (microstomia) – can make dental hygiene difficult.
- Telangiectasia.
- ‘Salt and pepper’ appearance of skin, due to areas of hypopigmentation and hyperpigmentation.
- Dry or itchy skin; reduced hair over affected skin areas.
Musculoskeletal features
- Joint pain and swelling.
- Myalgia (due to inflammatory myopathy).
- Restriction of joint movement, contractures and muscle atrophy due to skin sclerosis.
- Tendon friction rubs – palpable/audible over the flexor/extensor tendons of the hands, knees and ankles.
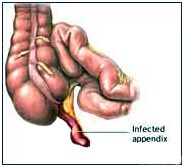
GI features
- Heartburn and reflux oesophagitis.
- Oesophageal scarring and dysphagia.
- Delayed gastric emptying – eg, fullness after meals.
- Reduced small bowel motility – can cause bacterial overgrowth, with bloating, malabsorption, diarrhoea and malnutrition.
- Constipation due to reduced colonic motility.
Pulmonary features
- Pulmonary fibrosis (interstitial lung disease):
- Occurs in as many as 75% of scleroderma patients, but only a few develop end-stage disease.
- Causes restrictive lung disease.
- Symptoms and signs: exertional dyspnoea, cough, coarse basal crackles.
- Pulmonary arterial hypertension (PAH):
- Occurs in about 10-15% of patients with scleroderma.
- A leading cause of death in SSc. The presence of PAH drastically reduces survival rate.
- Symptoms and signs: exertional dyspnoea, syncope, right ventricular strain features.
- Recent research has attempted to define predictive screening tools. These include monitoring lung function, ECG, urate levels, and N-terminal prohormone of brain natriuretic peptide (NT-proBNP); and by taking into account anti-centromere antibody (ACA) presence and history or presence of telangiectasia.
Management of GI symptoms
For upper GI symptoms:
- Maintain upright posture after meals; raise the head of the bed; limit alcohol.
- Proton pump inhibitors.
- May also need H2-receptor antagonists and pro-motility agents (metoclopramide or domperidone).
- Dilatation of oesophageal strictures if required.
For intestinal bacterial overgrowth and malabsorption:
- Cyclical antibiotics.
- Nutritional advice and nutritional supplements; rarely, parenteral nutrition is required.
For constipation:
- Dietary fibre and good fluid intake.
- Softening laxatives (such as lactulose) and/or soluble fibre (such as ispaghula).
Management of pulmonary disease
Pulmonary fibrosis (interstitial lung disease)
- Benefits of cyclophosphamide seem clear, but must be weighed against side-effects.
- Supportive treatment: prompt treatment of chest infections – oxygen if needed.
Pulmonary arterial hypertension (PAH)
- Drug treatment of PAH has improved recently and includes:
- Endothelin receptor antagonists – eg, bosentan or sitaxsentan.
- Vasodilators – eg, sildenafil.
- Prostaglandin derivatives – eg, iloprost (nebulised or intravenous) or epoprostenol (infusion).
- Supportive treatment – eg, oxygen.
Complications
GI complications
See also specific GI sections under ‘Clinical features’ and ‘Management’ headings.
- Malnutrition due to swallowing problems and other digestive issues.
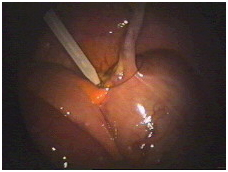
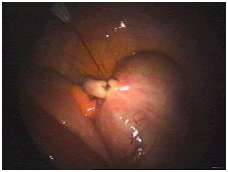
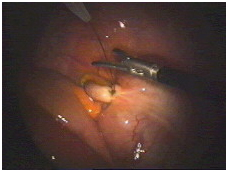
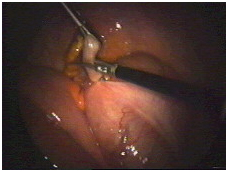
- ‘Watermelon stomach’ (gastric antral vascular ectasia):
- May cause anaemia and GI bleeding.
- May need endoscopic laser coagulation to prevent bleeding.
- Obstruction and pseudo-obstruction:
- Can occur due to reduced motility and bacterial overgrowth.
- Can be complicated by perforation and peritonitis.
- Pseudo-obstruction is treated initially by bowel rest and antibiotics.
- Laparotomy may be needed.
- Anorectal dysfunction:
- In some cases, the rectum and anus are involved, causing faecal incontinence.
- This may require surgery.
Scleroderma renal crisis
- A serious complication with features of accelerated hypertension.
- Can lead to renal failure if not treated promptly.
- Occurs in 5-10% of patients with scleroderma and is more common in those with diffuse or rapidly progressive disease.
- Presentation:
- Usually presents as accelerated hypertension with oliguria, headache, fatigue, oedema, rapidly rising serum creatinine levels, proteinuria and microscopic haematuria.
- Scleroderma renal crises can occur with apparently normal blood pressure, but the blood pressure is higher than baseline values – hence the importance of regular blood pressure monitoring.
- Treatment is with angiotensin-converting enzyme (ACE) inhibitors, plus dialysis if necessary.
- Testing patients with scleroderma for anti-RNA polymerase III antibodies may help identify at-risk patients.
Pulmonary complications
- Aspiration pneumonia from severe reflux.
- Respiratory muscle weakness if there is severe myositis or extensive skin disease involving the chest.
- Pneumothorax
Cardiac complications
- Many different cardiac abnormalities can be associated with SSc. These include:
- Microvascular coronary artery disease (with resultant myocardial ischemia).
- Myocardial fibrosis.
- Left ventricular (LV) systolic dysfunction, LV diastolic dysfunction.
- Pericarditis or pericardial effusion; these may cause cardiac impairment or congestive cardiac failure.
- Arrhythmias and conduction defects (including bradyarrhythmias and tachyarrhythmias).
- The wide variety of abnormalities makes it difficult to assess prevalence. It is likely that the subclinical cardiac involvement rates are very high.
- Treatment is according to the clinical features.
Other complications
- Erectile dysfunction.
- Depression.
- Osteoporosis – due to reduced blood flow.
- Hypothyroidism may be associated.
Treatments:
Management: general
There is no cure for SSc, and management consists of controlling symptoms and preventing complications.
Monitoring
Regular monitoring and reviews are aimed at early detection and treatment of complications. Monitoring includes:
- Regular review of symptoms.
- Blood pressure monitoring.
- Renal function monitoring.
- Lung function tests and chest CT scan.
- ECG and echocardiography.
Non-drug treatments
- Patient involvement and education:
- ‘Expert patient’ programmes and the Scleroderma Society.
- Awareness of urgent problems such as renal crisis or intestinal obstruction symptoms.
- Physiotherapy to promote joint mobility and muscle strength.
- Home exercises to maintain range of motion (such as gentle mouth, face and hand stretches).
- Avoid tobacco and maintain healthy weight.
- Nutritional advice, and supplements if needed.
- For Raynaud’s phenomenon:
- Prevention – avoid cold and trauma; use warm clothing or heated clothing.
- For an attack – warm the body, hands and feet gently (the skin may be numb and unable to feel if the heat source is too hot); use gentle arm movements or gentle massage to help restore circulation.
- Occupational therapists – for adaptations to assist in daily living.
- Camouflage products – for cosmetic help with skin changes.