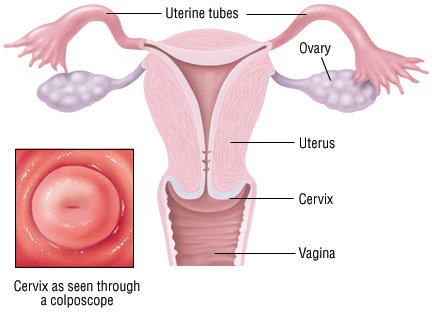
The cervix is a tubelike channel that connects the uterus to the vagina. Cervical polyps are growths that usually appear on the cervix where it opens into the vagina. Polyps are usually cherry-red to reddish-purple or grayish-white. They vary in size and often look like bulbs on thin stems. Cervical polyps are usually not cancerous (benign) and can occur alone or in groups. Most polyps are small, about 1 centimeter to 2 centimeters long. Because rare types of cancerous conditions can look like polyps, all polyps should be removed and examined for signs of cancer.
The cause of cervical polyps is not well understood, but they are associated with inflammation of the cervix. They also may result from an abnormal response to the female hormone estrogen.
Cervical polyps are relatively common, especially in women older than 20 who have had at least one child. They are rare in girls who have not started menstruating. There are two types of cervical polyps:
- Ectocervical polyps can develop from the outer surface layer cells of the cervix. They are more common in postmenopausal women.
- Endocervical polyps develop from cervical glands inside the cervical canal. Most cervical polyps are endocervical polyps, and are more common in premenopausal women.
Symptoms
Cervical polyps may not cause any symptoms. However, you may experience:
- Discharge, which can be foul-smelling if there is an infection
- Bleeding between periods
- Heavier bleeding during periods
- Bleeding after intercourse
Diagnosis
If you have a cervical polyp, you probably won’t be able to feel it or see it. Cervical polyps are discovered during routine pelvic exams or evaluations for bleeding or while getting a Pap test.
Expected Duration
Sometimes a polyp will come off on its own during sexual intercourse or menstruation. However, most polyps need to be removed to treat any symptoms and to evaluate the tissue for signs of cancer, which is rare.
 |
Prevention
Visit your doctor for an annual Pap test and for regular pelvic exams. A direct examination is the best way to identify cervical polyps.
Treatment
Cervical polyps are removed surgically, usually in a doctor’s office. The doctor will use a special instrument, called a polyp forceps, to grasp the base of the polyp stem and then gently pluck the polyp with a gentle, twisting motion. Bleeding is usually brief and limited. Nonprescription, mild pain medication such as acetaminophen (Tylenol and others) or ibuprofen (Advil, Motrin and others) can help to relieve discomfort or cramping during or after the procedure.
The polyp or polyps are sent to a laboratory for examination. You may receive antibiotics if the polyp shows signs of infection. If the polyp is cancerous, treatment will depend on the extent and type of cancer.
Large polyps and polyp stems that are very broad usually need to be removed in an operating room using local, regional or general anesthesia. You will not need to stay in the hospital overnight. Cervical polyps may grow in the future from different areas of the cervix, usually not from the original site. Regular pelvic examination will help to identify and treat polyps before they cause symptoms.
When To Call a Professional
If you experience vaginal discharge, bleeding after intercourse, or bleeding between periods, make an appointment to see your doctor as soon as possible for a pelvic exam.
Prognosis
The outlook is excellent. The vast majority of cervical polyps are not cancerous. Once removed, polyps usually don’t come back.