A rotator cuff injury can be painful and reduce range of motion.
Symptoms
The pain associated with a rotator cuff injury may:
- Be described as a dull ache deep in the shoulder
- Disturb sleep, particularly if you lie on the affected shoulder
- Make it difficult to comb your hair or reach behind your back
- Be accompanied by arm weakness
When to see a doctor
Shoulder pain that is short-lived may be evaluated by your family doctor. See your doctor right away if you have a sudden loss of motion after an injury — you could have a substantial rotator cuff tear. If you have pain lasting longer than a few weeks or you’ve been formally diagnosed with a rotator cuff tear, you need to be seen by a shoulder specialist, because some of the surgical procedures are time sensitive.
Causes
Rotator cuff disease may be the result of either a substantial injury to the shoulder or to progressive degeneration or wear and tear of the tendon tissue. Repetitive overhead activity, heavy lifting over a prolonged period of time, and the development of bone spurs in the bones around the shoulder may irritate or damage the tendon.
Risk factors
The following factors may increase your risk of having a rotator cuff injury:
- Age. As you get older, your risk of a rotator cuff injury increases. Rotator cuff tears are most common in people older than 40.
- Certain sports. Athletes who regularly use repetitive arm motions, such as baseball pitchers, archers and tennis players, have a greater risk of having a rotator cuff injury.
- Construction jobs. Occupations such as carpentry or house painting require repetitive arm motions, often overhead, that can damage the rotator cuff over time.
- Family history. There may be a genetic component involved with rotator cuff injuries as they appear to occur more commonly in certain families.
Treatments
Without treatment, rotator cuff disease may lead to permanent stiffness or weakness and may result in progressive degeneration of the shoulder joint.
Although resting your shoulder is necessary for your recovery, keeping your shoulder immobilized for a prolonged time can cause the connective tissue enclosing the joint to become thickened and tight (frozen shoulder).
Conservative treatments — such as rest, ice and physical therapy — sometimes are all that’s needed to recover from a rotator cuff injury. If your injury is severe and involves a complete tear of the muscle or tendon, you might need surgery.
Injections
If conservative treatments haven’t reduced your pain, your doctor might recommend a steroid injection into your shoulder joint, especially if the pain is interfering with your sleep, daily activities or exercise. While such shots are often helpful, they should be used judiciously, as they can contribute to weakening of the tendon.
Therapy
Physical therapy exercises can help restore flexibility and strength to your shoulder after a rotator cuff injury. Sometimes it is possible to eliminate pain and restore function without surgery.
Surgery
Many different types of surgeries are available for rotator cuff injuries, including arthroscopic tendon repair, open tendon repair, bone spur removal, tendon transfer and shoulder replacement.
-
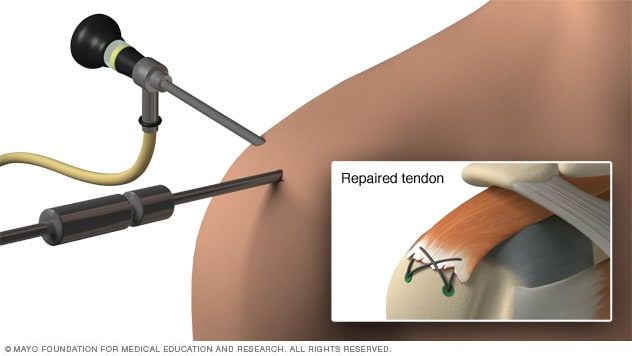
Arthroscopic rotator cuff repair
Arthroscopic tendon repair
In this procedure, surgeons insert a tiny camera (arthroscope) and tools through small incisions to reattach the torn tendon to the bone. Arthroscopic tendon repair can provide restoration of the patient’s normal anatomy with a relatively pain-free procedure.
-
Open repair of rotator cuff
- Open tendon repair
In some situations, an open tendon repair may be a better option. In these types of surgeries, your surgeon works through a larger incision to reattach the damaged tendon to the bone. Open tendon repairs typically have a longer recovery time than that seen with more minimally invasive procedures done arthroscopically.
If an overgrowth of bone is irritating your rotator cuff, this excess bone can be removed and the damaged portion of the tendon can be smoothed. This procedure is often performed using arthroscopy, where a fiber-optic camera and special tools are inserted through tiny incisions.
Tendon transfer
If the torn tendon is too damaged to be reattached to the arm bone, surgeons may decide to use a nearby tendon as a replacement.
- Reverse shoulder replacement
-
Shoulder replacement
Massive rotator cuff injuries may require shoulder replacement surgery. To improve the artificial joint’s stability, an innovative procedure (reverse shoulder arthroplasty) installs the ball part of the artificial joint onto the shoulder blade and the socket part onto the arm bone.



















