What is laryngeal cancer?
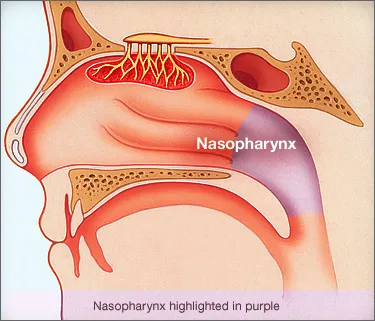
Laryngeal cancer occurs when cancerous (malignant) cells form on the tissues of the larynx, or voice box. The larynx contains the vocal folds. The vocal folds vibrate. This makes sound when air is directed against them. A person’s voice is heard when this sound echoes through the throat, mouth, and nose.
What are some signs or symptoms of laryngeal cancer?
A person with laryngeal cancer may notice:
- hoarseness or change in his or her voice
- difficulty swallowing
- a lump in the throat
- bad cough or chest infection
- shortness of breath
- bad breath (halitosis)
- weight loss
- prolonged earache
How is laryngeal cancer diagnosed?
You should visit a doctor if you have any of the above-mentioned symptoms. A doctor will feel your throat for lumps. He or she will also look down your throat with an endoscope, a tube with a special light, to see your larynx. This procedure is called a laryngoscopy. The doctor may need to cut out a small piece of tissue, if the larynx has tissue that does not look normal. The doctor will look at the tissue under a microscope to see if it contains any cancer cells. This procedure is called a biopsy, and it is the only way to diagnose cancer.
What treatments are available for individuals with laryngeal cancer?
One or more of the following approaches may be used depending on the size, location, and time of cancer detection:
- radiation therapy
- chemotherapy
- partial removal of the larynx (laryngectomy)
- total laryngectomy
In these cases, the person may still be able to produce voice. However, the person’s voice may not be the same because of removing parts of the larynx, changes to laryngeal tissue from radiation or chemotherapy, or removal of nearby neck muscles (to prevent or stop the spread of the cancer).
In extreme cases, total laryngectomy, with or without radiation therapy or chemotherapy, may be the only life-saving solution.
Patients who have undergone radiation treatment may have:
- dry and/or red skin at the site of the treatment
- sore throat
- dry mouth (xerostomia)
- sensitive mouth
- mouth sores
- difficulty swallowing
- decreased taste
- fatigue
- breathing difficulties from swelling
Patients who have received chemotherapy, often for the treatment of metastasized cancer (i.e., cancer that has spread), may have:
- nausea or vomiting
- increased chance of infection
- bleeding or bruising
- fatigue
- shortness of breath
These side effects often stop after the chemotherapy is discontinued.
Speech-language pathologists (SLPs) play an important role both before and after surgery.
What is a laryngectomy?
A laryngectomy is the removal of the voice box (larynx) from the neck, usually because of cancer. During this operation, a new route for breathing is surgically created. The end of the windpipe (trachea) is connected to a hole (stoma) made in the neck. Rather than using the mouth and the nose, the person will breathe through this hole.
Because the patient with the laryngectomy breathes through a stoma, the air inhaled into the lungs is no longer warmed or moisturized by structures of the nose and mouth. As a result, the breathing tubes can become irritated and create a thick mucus. This mucus may also crust on the stoma and require routine removal. The patient may benefit from humidifiers and a cover to protect the stoma.
What causes laryngeal cancer?
The following may increase your risk of laryngeal cancer:
- heavy smoking and drinking
- poor eating habits-not enough vitamins from fruits and vegetables
- weakened immune system
- exposure to chemicals and certain substances (e.g., wood dust, paint fumes, soot)
- acid reflux