What is gum disease?
Periodontal disease (gum disease) is a chronic bacterial infection of the gums and bone supporting the teeth. It is a major cause of tooth loss in adults. However, because gum disease is usually painless, you may not even know you have it. Gum disease is caused by plaque bacteria which form a sticky film on the tooth surface. These plaque bacteria release toxins that can damage the gums. As the amount of plaque increases the saliva in your mouth can begin to mineralise the plaque to form tartar (calculus). These hard deposits on the roots of the teeth only serve to promote more plaque formation and further damage to the gums.
Types of Gum disease
There are two main types of gum disease- gingivitis and periodontitis. Gingivitis is very common and may affect up to 70% of the population. Periodontitis affects around 30% of adults over age of 30. Both these infections can be treated and controlled, but the earlier they are diagnosed and managed, generally the better the prognosis for your teeth.

A patient with generalised gingivitis. Note the red, swollen, inflammed gum tissues around the teeth. These gums bleed easily on brushing.
Diagnosis and treatment
Diagnosis and treatment of periodontitis in its early stages will significantly enhance the prognosis for the dentition. If you have not had a periodontal screening examination with your dentist in the last 12 months, make it a priority. Remember, most patients who present with periodontitis are completely unaware of a gum problem being present in their mouth because it rarely causes pain until it becomes very severe, by which time it may be too late to save your teeth.
What are the warning signs of gum disease?
Periodontal disease is typically painless and often the signs are subtle. Some of the symptoms may include:
- gums that bleed easily with brushing or flossing
- red, swollen or tender gums
- pus between gums and teeth
- gums that pull away from the teeth
- persistent bad breath
- loose or separating teeth
- a change in the way your teeth fit together when you bite
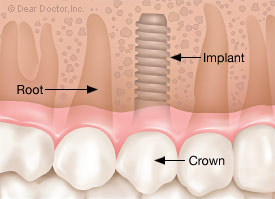
 Normal healthy gumsHealthy gums and bone anchor teeth firmly in place. Normal healthy gumsHealthy gums and bone anchor teeth firmly in place. |
 PeriodontitisUnremoved plaque hardens into calculus (tartar), As plaque and calculus continue to build up, the gums begin to recede( pull away) from the teeth, and pockets form between the teeth and gums. PeriodontitisUnremoved plaque hardens into calculus (tartar), As plaque and calculus continue to build up, the gums begin to recede( pull away) from the teeth, and pockets form between the teeth and gums. |
 Advanced PeriodontitisThe gums recede further, destroying more bone and the periodontal ligament. Even healthy teeth may become loose and need to be extracted Advanced PeriodontitisThe gums recede further, destroying more bone and the periodontal ligament. Even healthy teeth may become loose and need to be extracted |
An increasing amount of research also suggests that there is evidence linking chronic periodontal disease to conditions such as coronary heart disease, diabetes and respiratory disease. Moreover, current research suggests that if you have periodontal disease during pregnancy you may be significantly more likely to have a baby born prematurely or with a low birth weight. Keeping your gums healthy will ensure a better chance of good general health.

A case of advanced Periodontitis. Very swollen gums, loose teeth, staining and heavy plaque and calculus deposits on all the teeth.

Heavy calculus (tartar) deposits on the inside aspect of the lower incisor teeth in a patient with periodontitis.

Patient with advanced periodontitis showing severe loss of bone and gum recession.
Risk Factors for Gum Disease
The main cause of periodontal disease is bacterial plaque. Oral bacteria form a sticky, colourless film on your teeth. These bacteria release various toxic by-products which irritate your gum tissues. While plaque bacteria are the main cause of periodontal disease there are other factors, such as those outlined below, that can also affect the health of your gums.
Smoking and Tobacco Use
The use of tobacco is linked with many serious illnesses such as cancer, lung disease and heart disease, as well as numerous other health problems. Smoking also increases the risk of periodontal disease and recent research has shown that tobacco use may be one of the most significant risk factors in the development and progression of periodontal disease. Smoking also reduces the ability of your gums to heal properly following treatment, which may mean a less successful treatment outcome. Patients who smoke are also more prone to developing post operative infections following treatment. For these reasons all patients are encouraged to quit smoking as part of their periodontal therapy.
Genetics
Recent studies suggest that approximately 30% of the population may be genetically more susceptible to developing gum disease. Thus, some individuals are more prone to periodontal disease. Often the susceptibility to periodontal infection can be traced though families. Patients with a susceptibility to periodontal disease may require more intensive maintenance and more frequent recall for hygiene treatment.
Pregnancy & Puberty
At certain times such as puberty, menopause, menstruation and pregnancy your gum tissues may be more susceptible to irritation and infection. During these particular times your body experiences specific hormonal changes which can affect your gum tissues. Your gums may become more sensitive and at times react strongly to the hormonal fluctuations. Recent research also suggests that pregnant women with chronic gum disease are up to seven times more likely to deliver pre-term, low-birth-weight babies.
Grinding or Clenching your Teeth
Tooth grinding typically occurs at night while you are asleep and is also know as bruxism. Your jaw joint may click on opening or may be painful at times. If you wake up with frequent headaches and show wear on your teeth, you may be grinding your teeth. Tooth grinding may worsen your gum health if you have pre-existing periodontal disease.
Diabetes
Diabetes is one of the main risk factors in periodontal disease. Diabetics are generally more prone to developing infections, including periodontal disease. Periodontal disease is often more severe in diabetics and can be more difficult to treat, depending you the level of diabetic control.
Stress
Chronic stress can have a negative effect of you body’s immune system. This may in turn make you more susceptible to periodontal disease as it can make it more difficult for the body to fight off infection.
Medications
Certain drugs, such as antidepressants, oral contraceptives and some heart medicines, can have an effect on your oral health. You should always inform your dental professional of the medications you are taking so that these can be taken into consideration.
Poor Nutrition
A diet low in important vitamins and nutrients can compromise the body’s immune system and make it harder for the body to fight off infection. One of the more common conditions is iron deficiency. Deficiencies such as this can worsen the condition of your gums.
Other Systemic Diseases
Certain diseases may worsen your gum disease by interfering with the way your body’s defences deal with infection. Some examples include uncontrolled diabetes, radiation therapy, chemotherapy, corticosteroid use.
Maintaining Periodontal Health
After your gum disease has been diagnosed and treated, ongoing supportive treatment to maintain your periodontal heath will be recommended.
Supportive Periodontal Therapy
This consists of structured and regular hygiene treatment that is aimed at preventing and reducing the possibility of the recurrence and progression of periodontal disease. Each patient will have specific maintenance requirements which will need to be professionally tailored to their needs. The Oral Hygiene Spa at the Institute of Dental Implants & Periodontics provides the highest level of periodontal maintenance under the specialist supervision of a Periodontist.
Good Oral Hygiene Habits
As part of your periodontal treatment you will be given careful oral hygiene instruction and shown the right ‘tools’ to use. It is important that you regularly remove plaque bacteria through brushing, flossing, and regular professional cleaning. Good oral hygiene will leave you with a fresh, healthy mouth and reduce your risk of further gum disease. There are other risk factors that may compromise your periodontal health such as stress, diabetes, genetics, and pregnancy. These other factors may be transient, but should be discussed with your dental health professional.












 Normal healthy gumsHealthy gums and bone anchor teeth firmly in place.
Normal healthy gumsHealthy gums and bone anchor teeth firmly in place. PeriodontitisUnremoved plaque hardens into calculus (tartar), As plaque and calculus continue to build up, the gums begin to recede( pull away) from the teeth, and pockets form between the teeth and gums.
PeriodontitisUnremoved plaque hardens into calculus (tartar), As plaque and calculus continue to build up, the gums begin to recede( pull away) from the teeth, and pockets form between the teeth and gums. Advanced PeriodontitisThe gums recede further, destroying more bone and the periodontal ligament. Even healthy teeth may become loose and need to be extracted
Advanced PeriodontitisThe gums recede further, destroying more bone and the periodontal ligament. Even healthy teeth may become loose and need to be extracted