Your spinal column is made up of a series of bones (vertebrae) stacked onto each other. From top to bottom, the column includes seven bones in the cervical spine, 12 in the thoracic spine, and five in the lumbar spine, followed by the sacrum and the coccyx at the base. These bones are cushioned by disks. The disks protect the bones by absorbing the shocks from daily activities like walking, lifting, and twisting.
Each disk has two parts: a soft, gelatinous inner portion and a tough outer ring. Injury or weakness can cause the inner portion of the disk to protrude through the outer ring. This is known as a slipped, herniated, or prolapsed disk. This causes pain and discomfort. If the slipped disk compresses one of your spinal nerves, you may also experience numbness and pain along the affected nerve. In severe instances, you may require surgery to remove or repair the slipped disk.

Symptoms of a slipped disk?
You can have a slipped disk in any part of your spine, from your neck to your lower back. The lower back is one of the more common areas for slipped disks. Your spinal column is an intricate network of nerves and blood vessels. A slipped disk can place extra pressure on the nerves and muscles around it.
Symptoms of a slipped disk include:
- pain and numbness, most commonly on one side of the body
- pain that extends to your arms or legs
- pain that worsens at night or with certain movements
- pain that worsens after standing or sitting
- pain when walking short distances
- unexplained muscle weakness
- tingling, aching, or burning sensations in the affected area
The types of pain can vary from person to person. See your doctor if your pain results in numbness or tingling that affects your ability to control your muscles.
What causes slipped disks?
A slipped disk occurs when the outer ring becomes weak or torn and allows the inner portion to slip out. This can happen with age. Certain motions may also cause a slipped disk. A disk can slip out of place while you are twisting or turning to lift an object. Lifting a very large, heavy object can place great strain on the lower back, resulting in a slipped disk. If you have a very physically demanding job that requires a lot of lifting, you may be at increased risk for slipped disks.
Overweight individuals are also at increased risk for a slipped disk because their disks must support the additional weight. Weak muscles and a sedentary lifestyle may also contribute to the development of a slipped disk.
As you get older, you are more likely to experience a slipped disk. This is because your disks begin to lose some of their protective water content as you age. As a result, they can slip more easily out of place. They are more common in men than women.
How are slipped disks treated?
Treatments for a slipped disk range from conservative to surgical. The treatment typically depends on the level of discomfort you’re experiencing and how far the disk has slipped out of place.
Most people can relieve slipped disk pain using an exercise program that stretches and strengthens the back and surrounding muscles. A physical therapist may recommend exercises that can strengthen your back while reducing your pain.
Taking over-the-counter pain relievers and avoiding heavy lifting and painful positions can also help.
While it may be tempting to refrain from all physical activity while you’re experiencing the pain or discomfort of a slipped disk, this can lead to muscle weakness and joint stiffness. Instead, try to remain as active as possible through stretching or low-impact activities such as walking.
If your slipped disk pain does not respond to over-the-counter treatments, your doctor may prescribe stronger medications. These include:
- muscle relaxers to relieve muscle spasms
- narcotics to relieve pain
- nerve pain medications like gabapentin or duloxetine
Your doctor may recommend surgery if your symptoms do not subside in six weeks or if your slipped disk is affecting your muscle function. Your surgeon may remove the damaged or protruding portion of the disk without removing the entire disk. This is called a microdiskectomy.
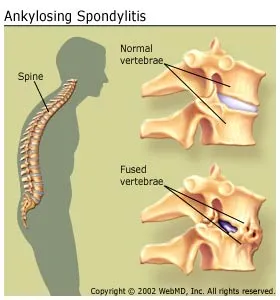
In more severe cases, your doctor may replace the disk with an artificial one or remove the disk and fuse your vertebrae together. This procedure, along with a laminectomy and spinal fusion, adds stability to your spinal column.
What is the outlook for someone with a slipped disk?
Most people with a slipped disk respond well to conservative treatment. Within six weeks their pain and discomfort will gradually lessen.
Is it possible to prevent a slipped disk?
It may not be possible to prevent a slipped disk, but you can take steps to reduce your risk of developing a slipped disk. These steps include:
- Use safe lifting techniques: Bend and lift from your knees, not your waist.
- Maintain a healthy weight.
- Do not remain seated for long periods; get up and stretch periodically.
- Do exercises to strengthen the muscles in your back, legs, and abdomen.