What is carpal tunnel syndrome?
Carpal tunnel syndrome is numbness, tingling, weakness, and other problems in your hand because of pressure on the median nerve in your wrist.his is a common occurrence among IT professionals and sedentary workers who are working on laptops for long duration.
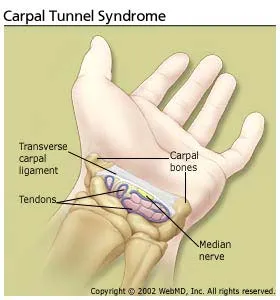
The median nerve and several tendons run from your forearm to your hand through a small space in your wrist called the carpal tunnel . The median nerve controls movement and feeling in your thumb and first three fingers (not your little finger).
What causes carpal tunnel syndrome?
Pressure on the median nerve causes carpal tunnel syndrome. This pressure can come from swelling or anything that makes the carpal tunnel smaller. Many things can cause this swelling, including:
- Illnesses such as hypothyroidism, rheumatoid arthritis, and diabetes.
- Making the same hand movements over and over, especially if the wrist is bent down (your hands lower than your wrists), or making the same wrist movements over and over.
- Pregnancy.
What are the symptoms?
Carpal tunnel syndrome can cause tingling, numbness, weakness, or pain in the fingers or hand. Some people may have pain in their arm between their hand and their elbow.
Symptoms most often occur in the thumb, index finger, middle finger, and half of the ring finger. If you have problems with your other fingers but your little finger is fine, this may be a sign that you have carpal tunnel syndrome. A different nerve gives feeling to the little finger.
You may first notice symptoms at night. You may be able to get relief by shaking your hand.
How is it treated?
Mild symptoms usually can be treated with home care. You can:
- Stop activities that cause numbness and pain. Rest your wrist longer between activities.
- Ice your wrist for 10 to 15 minutes 1 or 2 times an hour.
- Try taking nonsteroidal anti-inflammatory drugs (NSAIDs)to relieve pain and reduce swelling.
- Wear a wrist splint at night. This takes pressure off your median nerve.
The sooner you start treatment, the better your chances of stopping symptoms and preventing long-term damage to the nerve.
You also may need medicine for carpal tunnel syndrome or for a health problem that made you likely to get carpal tunnel syndrome.
Surgery is an option. But it’s usually used only when symptoms are so bad that you can’t work or do other things even after several weeks to months of other treatment.
How can you keep carpal tunnel syndrome from coming back?
To keep carpal tunnel syndrome from coming back, take care of your basic health. Stay at a healthy weight. Don’t smoke. Exercise to stay strong and flexible. If you have a long-term health problem, such as arthritis or diabetes, follow your doctor’s advice for keeping your condition under control.
You can also try to take good care of your wrists and hands:
- Try to keep your wrist in a neutral position.
- Use your whole hand-not just your fingers-to hold objects.
- When you type, keep your wrists straight, with your hands a little higher than your wrists. Relax your shoulders when your arms are at your sides.
- If you can, switch hands often when you repeat movements.