What is pernicious anemia?
Anemia is a condition in which the body does not have a sufficient number of red blood cells or hemoglobin. Hemoglobin is present within red blood cells and is important for carrying oxygen to all tissues of the body. In males, anemia is typically defined as hemoglobin level of less than 13.5 gram/100ml, while in women, a hemoglobin level of less than 12.0 gram/100ml is considered to be indicative of anemia. These definitions may vary slightly depending on the source and the laboratory reference used. Pernicious is a term that means destructive, injurious or deadly.
Anemia can result from disruptions in the production of red blood cells or hemoglobin as well as from an increased destruction of red blood cells or loss of blood.
Pernicious anemia is a disease where large, immature, nucleated cells (megaloblasts, which are forerunners of red blood cells) circulate in the blood, and do not function as blood cells; it is a disease caused by impaired uptake of vitamin B-12 due to the lack of intrinsic factor (IF) in the gastric mucosa. It was termed “pernicious” because before it was learned that vitamin B-12 could treat the anemia, most people that developed the disease died from it.
Pernicious anemia is due to an inability to absorb vitamin B-12 (also known as cobalamin or Cbl) from the gastrointestinal tract. Humans get vitamin B-12 from animal products; both meat and dairy products are dietary sources of vitamin B-12. The body is able to store vitamin B-12 for a long time, so inadequate dietary intake must persist for years before a true deficiency of vitamin B-12 is reached. Therefore, the symptoms of pernicious anemia usually do not appear for years. While pernicious anemia is most commonly diagnosed in adults with an average age of 60, a rare, congenital (inborn) type of pernicious anemia has been described.
As with other causes of anemia, symptoms related to decreased oxygen-carrying capacity of the blood can include tiredness and shortness of breath. Vitamin B-12 deficiency also interferes with the function of the nervous system, and symptoms due to nervous system damage may be apparent even before the anemia is discovered.
Pernicious anemia facts
- Pernicious anemia is defined as a type of vitamin B12 deficiency that results from impaired uptake of vitamin B-12 due to the lack of a substance known as intrinsic factor (IF) produced by the stomach lining.
- Pernicious anemia is a condition caused by too little vitamin B12 in the body. It is one form of vitamin B12 deficiency anemia.
- Vitamin B12 helps the body make healthy red blood cells and helps keep nerve cells healthy. It is found in animal foods, including meat, fish, eggs, milk, and other dairy products.
- The most common cause of pernicious anemia is the loss of stomach cells that make intrinsic factor. Intrinsic factor helps the body absorb vitamin B12 in the intestine. The loss of parietal cells may be due to destruction by the body’s own immune system.
- Pernicious anemia can cause permanent damage to nerves and other organs if it goes on for a long time without being treated. It also raises the risk for developing stomach cancer.
- Common signs and symptoms of vitamin B12 deficiency, seen in pernicious anemia are:
- Feeling tired and weak
- Tingling and numbness in hands and feet
- A bright red, smooth tongue
- Pernicious anemia is diagnosed using family history and medical history, a physical exam, and diagnostic tests and procedures.
- Pernicious anemia is easy to treat with vitamin B12 pills or shots as well as dietchanges. Life-long treatment is needed.
- Complications caused by untreated pernicious anemia may be reversible with treatment.
- Doctors don’t know how to prevent pernicious anemia that is caused by the immune system destroying stomach cells.
- Eating foods high in vitamin B12 and folic acid can help prevent vitamin B12 deficiency caused by a poor diet.
What causes pernicious anemia?
Pernicious anemia is considered to be an autoimmune disease, in which the body’s own immune system mistakenly damages its own tissues. It is believed that the decreased absorption of vitamin B-12 from the gastrointestinal tract in pernicious anemia results from the presence of an autoantibody against intrinsic factor (IF), a protein made in the stomach that is necessary for the absorption of vitamin B-12. Normally, vitamin B-12 binds to intrinsic factor in the stomach, and this facilitates its absorption by the small intestine further along in the digestive process. Along with the autoimmune process that attacks the IF protein and lowers IF levels in stomach secretions, another autoimmune reaction against the stomach lining cells also occurs, resulting in a form of inflammation known as chronic atrophic gastritis.
Pernicious anemia is sometimes associated with other autoimmune diseases such as Graves’ disease, Hashimoto’s thyroiditis and vitiligo (depigmentation or blanching of skin areas)
What are the symptoms of vitamin B-12 deficiency/ pernicious anemia?
As discussed previously, true pernicious anemia results from an autoimmune condition that impairs absorption of dietary vitamin B-12, resulting in vitamin B-12 deficiency. Vitamin B-12 deficiency of any cause, including pernicious anemia, will result in anemia and neurologic symptoms. Because the body has large stores of vitamin B-12, a deficiency takes many years to establish.
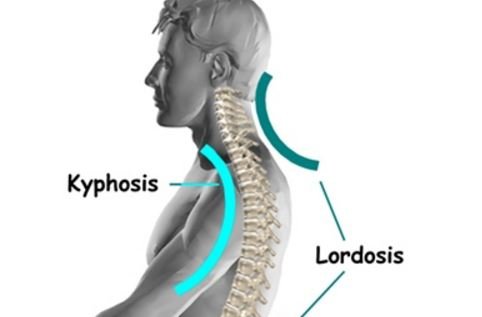
Vitamin B-12 deficiency affects the nervous system, leading to a variety of symptoms. Sometimes, these may be apparent before symptoms related to the anemia. Neurological symptoms vary and may be nonspecific (meaning that these are symptoms that can be caused by a number of different conditions). Feelings of numbness, tingling, weakness, lack of coordination, clumsiness, impaired memory, and personality changes can all occur. Both sides of the body are usually affected, and the legs are typically more affected than the arms. A severe deficiency can result in more serious neurological symptoms, including severe weakness, spasticity, paraplegia, and fecal and urinary incontinence.
Symptoms of anemia are due to the reduced oxygen-carrying capacity of the blood. Shortness of breath, fatigue, dizziness, and pale skin can all occur with anemia. In anemia, the heart is placed under stress since it has to work harder to deliver enough oxygen to body tissues. This can result in heart murmurs, fast heartbeats, arrhythmias, an enlarged heart (cardiomegaly), or even heart failure. It is important to note that not all people who have vitamin B-12 deficiency and neurological symptoms also will have anemia.
A deficiency of vitamin B-12 also can alter the surface of the tongue, making it appear shiny or smooth.
Finally, sometimes pernicious anemia is diagnosed in a patient with no symptoms. In these cases, it is usually found incidentally when blood tests are ordered for another reason.
What is the treatment for pernicious anemia and vitamin B-12 deficiency?
The symptoms of pernicious anemia and vitamin B-12 deficiency can be treated by replenishing the vitamin B-12 supply in the body. If a condition other than pernicious anemia is responsible for vitamin B-12 deficiency, treatment also must be directed at the underlying condition. Symptoms of vitamin B-12 deficiency may be improved after just a few days of medical treatment.
Vitamin B-12 is typically given as an intramuscular injection (shot). An injection of 1000 micrograms (1 mg) of vitamin B-12 is generally given every day for one week, followed by 1 mg every week for four weeks and then 1 mg every month thereafter.
Alternative treatments for pernicious anemia include high-dose oral vitamin B-12, since a lower-efficiency absorption system for vitamin B-12 exists in the intestine that does not require the presence of IF. However, the oral dose required for this type of therapy (1 to 2 milligrams/day) is more than 200 times higher than the minimum daily vitamin B-12 requirement for adults and is significantly higher than that available in most standard multivitamins and B-12 supplements. Nasal spray and sublingual (under the tongue) preparations of vitamin B-12 also are available and are under investigation.