List of Hospitals which is giving treatments for International Patients under Global Treatments Services P. Ltd., Bangalore are given below:
Dumping syndrome is common after gastric surgery. It is a group of symptoms that may result from having part of your stomachremoved or from other surgery involving the stomach. The symptoms range from mild to severe and often subside with time. Although you may find dumping syndrome alarming at first, it is not life threatening. You can control it by making changes in what and how you eat. By controlling dumping syndrome, you will also be avoiding the foods that tend to make you gain weight.
After gastric surgery, it can be more difficult to regulate movement of food, which dumps too quickly into the small intestine. Eating certain foods makes dumping syndrome more likely. For example, refined sugars rapidly absorb water from the body, causing symptoms. Symptoms may also happen after eating dairy products and certain fats or fried foods.
An early dumping phase may happen about 30 to 60 minutes after you eat. Symptoms can last about an hour and may include:

Symptoms of an early phase happen because food is rapidly “dumping” into the small intestine. This may be due to factors such as these:
A late dumping phase may happen about 1 to 3 hours after eating. Symptoms may include:
The symptoms of this late phase may happen due to a rapid rise and fall in blood sugar levels. The cause of this rapid swing in blood sugar may be worse when eating sweets or other simple carbohydrates.
If you have not already been diagnosed with the dumping syndrome, and you have confusion, dizziness, rapid heartbeat, or fainting, get immediate medical help.
Many people find that taking steps like these greatly reduces symptoms of dumping syndrome.
Foods to avoid. Avoid eating sugar and other sweets such as:
Also avoid dairy products and alcohol. And avoid eating solids and drinking liquids during the same meal. In fact, don’t drink 30 minutes before and 30 minutes after meals.
Foods to eat. To help with symptoms, also try these tips:
How to eat. Here are some other ways to lessen symptoms of dumping syndrome:
It is important to manage dumping syndrome so you stay well-nourished and don’t lose too much weight. Talk to your health care provider about any symptoms you have and what else you can do. In some cases, medication or surgery may be needed to help correct the symptoms of dumping syndrome.
If you’ve received the news that your lung contains something “suspicious,” this may be a source of great distress. The first thing that may come to mind is a dreaded word: cancer. In many cases, though, a lung nodule turns out to be benign. This means that it isn’t cancer. A hard part is waiting and not knowing. Here’s information that may make your wait just a little bit easier.
A nodule is a “spot on the lung,” seen on an X-ray or computed tomography (CT) scan. In fact, a nodule shows up on about one in every 500 chest X-rays. Normal lung tissue surrounds this small round or oval solid overgrowth of tissue. It may be a single or solitary pulmonary nodule. Or, you may have multiple nodules.
Your lung nodule is more likely to be benign if:
A benign lung tumor is an abnormal growth of tissue that serves no purpose and is found not to be cancerous. Benign lung tumors may grow from many different structures in the lung.
Determining whether a nodule is a benign tumor or an early stage of cancer is very important. That’s because early detection and treatment of lung cancer can greatly enhance your survival.
Benign lung nodules and tumors usually cause no symptoms. This is why they are almost always found accidentally on a chest X-ray or CT scan. However, they may lead to symptoms like these:

The causes of benign lung tumors and nodules are poorly understood. But in general, they often result from problems like these:
Inflammation from infections such as:
Inflammation from noninfectious causes such as:
These are some of the more common types of benign lung tumors:
A pleural effusion is an unusualamount of fluid around the lung.There are many medicalconditions that can lead to it. Soeventhough your pleural effusionmay have to be drained, yourdoctor likely will target thetreatment at whatever caused it.
The pleura is a thin membranethat lines the surface of the lungsand the inside of the chest walloutside the lungs. In pleuraleffusions, fluid builds up in thespace between the layers of pleura.
Normally, only teaspoons of watery fluid are in the pleural space, allowingthe lungs to move smoothly within the chest cavity during breathing.
A wide range of things can cause a pleural effusion. Some of the morecommon ones are:
You might not have any. You’re more likely to have symptoms when a pleuraleffusion is moderate or large-sized, or if inflammation is present.
If you do have symptoms, they may include:

Doctors use the terms “transudative” and “exudative” to describe the two main types of pleural effusions:
Transudative: This pleural effusion fluid is similar to the fluid you normally have in your pleural space. It forms from liquid leaking across normal pleura. This type of pleural effusion rarely needs to be drained unless they are very large. Congestive heart failure is the most common cause of this type of effusion.
Exudative: This effusion forms from excess liquid, protein, blood, inflammatory cells or sometimes bacteria leaking across damaged blood vessels into the pleura. It may need to be drained, depending on its size and how much inflammation is involved. Among its causes are pneumonia and lung cancer.
Your doctor may need to treat only the medical condition that caused the pleural effusion. You would get antibiotics for pneumonia, for instance, or diuretics for congestive heart failure.
Large, infected, or inflamed pleural effusions often need to be drained to help you feel better and to prevent more problems. Procedures for treating pleural effusions include:
A cold or the flu runs its course in a couple weeks, if you’re lucky. After that, you’re back to normal. But sometimes you may get bronchitis, too.
That’s when your bronchial tubes, which carry air to your lungs, get infected and swollen. You end up with a nagging cough and a lot more mucus.
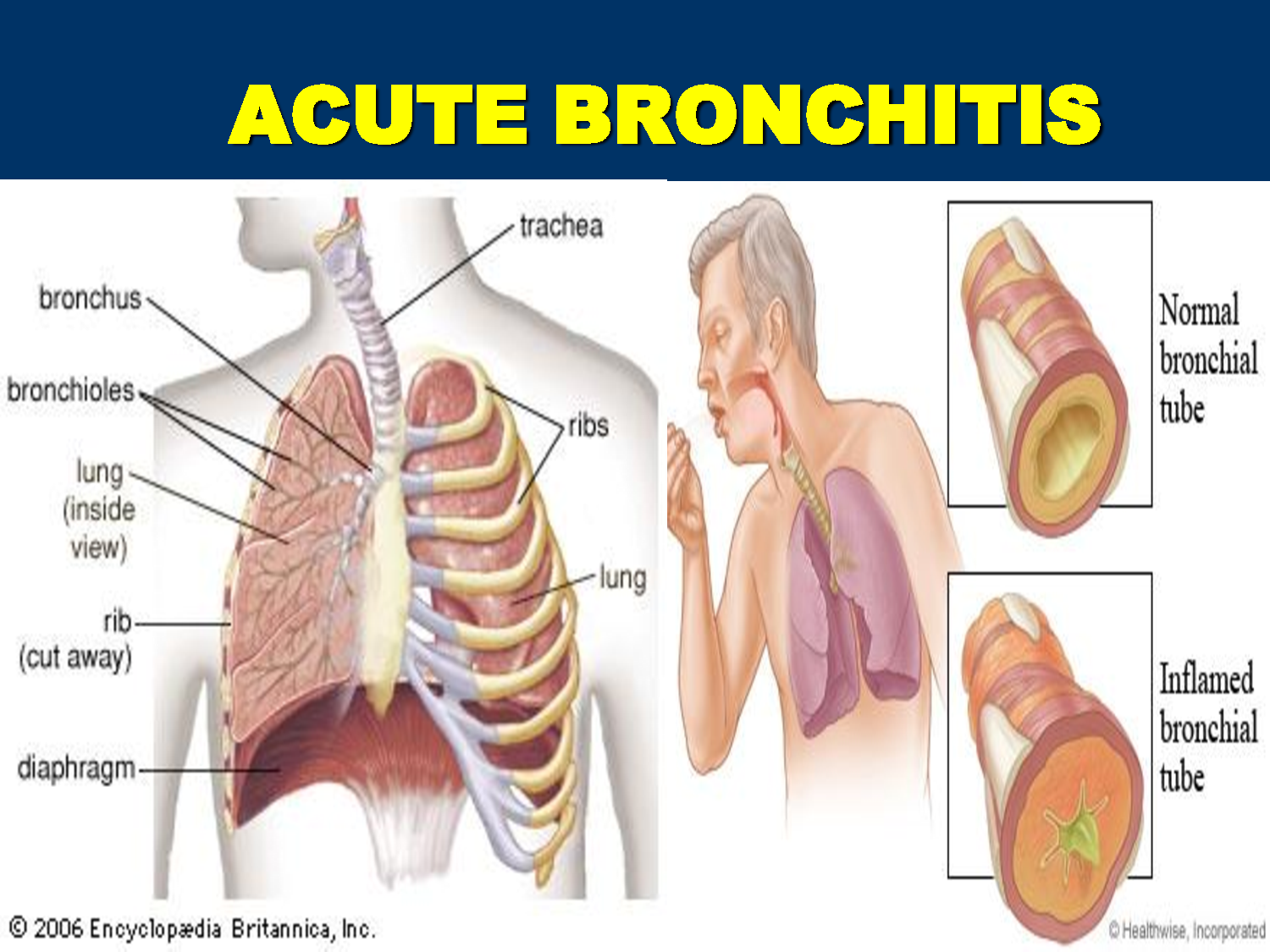

You can get bronchitis in other ways, too, and there are actually two types of it:
Most often, the same viruses that give you a cold or the flu also cause bronchitis. Sometimes, though, bacteria are to blame.
In both cases, as your body fights off the germs, your bronchial tubes swell and make more mucus. That means you have smaller openings for air to flow, which can make it harder to breathe.
If any of these things describe your situation, you have a bigger chance of getting bronchitis:
You’ll definitely have a cough, and you may have various problems with breathing, such as:
You may also:
Even after the other symptoms are gone, the cough can last for a few weeks while your bronchial tubes heal and the swelling goes down. If it goes on much longer than that, the problem might be something else.
Most of the time, bronchitis goes away on its own within a couple of weeks.
If yours is caused by bacteria (which is rare), your doctor may give you antibiotics.
If you have asthma, allergies, or you’re wheezing, she might suggest an inhaler. This helps open up your airways and makes it easier to breathe.
To ease your symptoms, you can:
Here are some ways to lower your chances of getting bronchitis:
The large intestine is the lowest section of your digestive tract. It includes your appendix, colon, and rectum. The large intestine completes the digestive process by absorbing water and passing waste (stool) to the anus.
Certain conditions can cause the large intestine to malfunction. One such condition is toxic megacolonor megarectum. Megacolon is a general term that means the abnormal dilation of the colon. Toxic megacolon is a term used to express the seriousness of the condition.
Toxic megacolon is rare. It’s a widening of the large intestine that develops within a few days and can be life-threatening. It can be a complication of inflammatory bowel disease (such as Crohn’s disease).
What causes toxic megacolon?
One of the causes of toxic megacolon is an inflammatory bowel disease (IBD). Inflammatory bowel diseases cause swelling and irritation in parts of your digestive tract. These diseases can be painful and cause permanent damage to your large and small intestines. Examples of IBDs are ulcerative colitis and Crohn’s disease. Toxic megacolon can also be caused by infections such as Clostridium difficile colitis.
Toxic megacolon occurs when inflammatory bowel diseases cause the colon to expand, dilate, and distend. When this happens, the colon is unable to remove gas or feces from the body. If gas and feces build up in the colon, your large intestine may eventually rupture.
Rupture of your colon is life-threatening. If your intestines rupture, bacteria that are normally present in your intestine release into your abdomen. This can cause a serious infection and even death.
It’s important to note that there are other types of megacolon. Examples include:
Although these conditions can expand and damage the colon, they’re not due to inflammation or infection.
When toxic megacolon occurs, the large intestines rapidly expand. Symptoms of the condition may come on suddenly and include:
Toxic megacolon is a life-threatening condition. If these symptoms develop, you should seek immediate medical attention.

The treatment of toxic megacolon usually involves surgery. If you develop this condition, you will be admitted to the hospital. You will receive fluids to prevent shock. Shock is a life-threatening condition that occurs when an infection in the body causes your blood pressure to decrease rapidly.
Once your blood pressure is stable, you’ll need surgery to correct toxic megacolon. In some cases, toxic megacolon may produce a tear or perforation in the colon. This tear must be repaired to prevent bacteria from the colon from entering the body.
Even if there’s no perforation, the tissue of the colon may be weakened or damaged and need removal. Depending on the extent of the damage, you may need to undergo a colectomy. This procedure involves either a complete or partial removal of the colon.
You’ll take antibiotics during and after the surgery. Antibiotics will help prevent a serious infection known as sepsis. Sepsis causes a severe reaction in the body that is often life-threatening.
If you develop toxic megacolon and promptly seek treatment at a hospital, your long-term outlook will be good. Seeking emergency medical treatment for this condition will help prevent complications, including:
If complications of toxic megacolon occur, your doctor may have to take serious measures. Complete removal of the colon may require you to have an ileostomy or ileoanal pouch-anal anastomosis (IPAA) put in place. These devices will remove feces from your body after your colon is removed.
Henoch-Schonlein purpura (HSP) is a disease involving inflammation of small bloodvessels. It most commonly occurs in children. The inflammationcauses blood vessels in the skin, intestines, kidneys, and joints to start leaking. The main symptom is a rash with numerous small bruises, which have a raised appearance, over the legs or buttocks.
Although HSP can affect people at any age, most cases occur in children between the ages of 2 and 11. It is more common in boys than girls. Adults with HSP are more likely to have more severe disease compared to children.
HSP usually ends after four to six weeks — sometimes with recurrence of symptoms over this period, but with no long-term consequences. If organs such as the kidneys and intestines are affected, treatment is often needed and it is important to have regular follow-up to prevent serious complications.

The exact cause of HSP is not known. The body’s immune system is believed to play a role in targeting the blood vessels involved. An abnormal immune response to an infection may be a factor in many cases. Approximately two-thirds of the cases of HSP occur days after symptoms of an upper respiratory tract infection develop.
Some cases of HSP have been linked to vaccinations for typhoid, cholera, yellow fever, measles, or hepatitis B; foods, drugs, chemicals, and insect bites. Some experts also say that HSP is associated with the colder weather of fall and winter.
The classic symptoms of HSP are rash, joint pain and swelling, abdominal pain, and/or related kidney disease, including blood in urine. Before these symptoms begin, patients may have two to three weeks of fever, headache, and muscular aches and pains. Rarely, other organs, such as the brain, heart, or lungs, may be affected.
Here are some key details about the symptoms of HSP:
Rash. The rash usually appears in all patients with HSP. The initial appearance may resemble hives, with small red spots or bumps on the lower legs, buttocks, knees, and elbows. But these change to appear more like bruises. The rash usually affects both sides of the body equally and does not turn pale on pressing.
Arthritis. Joint inflammation, involving pain and swelling, occurs in approximately three-quarters of cases, particularly affecting the knees and ankles. It usually lasts only a few days and does not cause any long-term, chronic joint problems.
Abdominal pain. In more than half of people with HSP, inflammation of the gastrointestinal tract may cause pain or cramping; it may also lead to loss of appetite, vomiting, diarrhea, and occasionally blood in the stool.
In some cases, patients may have abdominal pain before the rash appears. In rare cases, an abnormal folding of the bowel (intussusception) may cause a bowel blockage, which may require surgery to fix.
Kidney impairment. HSP can cause kidney problems, indicated by such signs as protein or blood in the urine. This is usually only discovered on urine testing, since it does not generally cause any discomfort.
In most patients, the kidney impairment is mild and goes away without any long-term damage. It’s important to monitor the kidney problems closely and make sure they clear up, since about 5% of patients may develop progressive kidney disease. About 1% may go on to develop total kidney failure.
The diagnosis of HSP may be clear when the typical rash, arthritis, and abdominal pain are present. A doctor may order some tests to rule out other diagnoses, confirm the diagnosis, and assess its severity.
Occasionally, when the diagnosis is uncertain, particularly if the only symptom is the classic rash, your doctor may perform biopsies of the skin or kidney. Urine and blood tests will likely be done to detect signs of kidney involvement and may need to be repeated during follow-up to monitor any changes in kidney function.
Although there is no specific treatment for HSP, you can use over-the-counter pain medicines, such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen for joint pain. In some cases, corticosteroid medication may be used.
The rash and joint pain will usually go away after four to six weeks without causing any permanent damage. Bouts of the rash may recur in approximately one-third of cases, but they are usually milder, do not involve joint and abdominal symptoms, and they clear up on their own.
Fecal incontinence is the inability to control bowel movements. It’s a common problem, especially among older adults.
Accidental bowel leakage is usually not a serious medical problem. But it can seriously interfere with daily life. People with bowel incontinence may avoid social activities for fear of embarrassment.
Many effective treatments can help people with bowel incontinence. These include:
Talking to your doctor is the first step toward freedom from bowel incontinence.
The most common cause of bowel incontinence is damage to the muscles around the anus (anal sphincters). Vaginal childbirth can damage the anal sphincters or their nerves. That’s why women are affected by accidental bowel leakage about twice as often as men.
Anal surgery can also damage the anal sphincters or nerves, leading to bowel incontinence.
There are many other potential causes of bowel incontinence, including:
More than one cause for bowel incontinence is frequently present. It’s also not unusual for bowel incontinence to occur without a clear cause.
Discussing bowel incontinence may be embarrassing, but it can provide clues for a doctor to help make the diagnosis. During a physical examination, a doctor may check the strength of the anal sphincter muscle using a gloved finger inserted into the rectum.
Stool testing. If diarrhea is present, stool testing may identify an infection or other cause.
Endoscopy. A tube with a camera on its tip is inserted into the anus. This identifies any potential problems in the anal canal or colon. A short, rigid tube (anoscopy) or a longer, flexible tube (sigmoidoscopy or colonoscopy) may be used.
Surgery may be recommended for people whose bowel incontinence is not helped by noninvasive treatments. The types of surgery include:
Anorectal manometry. Apressure monitor is inserted intothe anus and rectum. This allowsmeasurement of the strength ofthe sphincter muscles.
Endosonography. An ultrasoundprobe is inserted into the anus.This produces images that canhelp identify problems in the anal and rectal walls.
Nerve tests. These tests measure the responsiveness of the nervescontrolling the sphincter muscles. They can detect nerve damage thatcan cause bowel incontinence.
MRI defecography. Magnetic resonance imaging of the pelvis can beperformed, potentially while a person moves her bowels on a specialcommode. This can provide information about the muscles and supportingstructures in the anus, rectum, and pelvis.
Bowel incontinence is usually treatable. In many cases, it can be cured completely.
Recommended treatments vary acc
Medications. Try these medicines to reduce the number of bowel movements and the urge to move the bowels:
Methylcellulose can help make liquid stool more solid and easier to control. For people with a specific cause of diarrhea, such as inflammatory bowel syndrome, other medications may also help.
Exercises. Begin a program of regularly contracting the muscles used to control urinary flow (Kegel exercises). This builds strength in the pelvic muscles and may help reduce bowel incontinence.
Bowel training. Schedule bowel movements at the same times each day. This can help prevent accidents in between.
Biofeedback. A sensor is placed inside the anus and on the abdominal wall. This provides feedback as a person does exercises to improve bowel control.
Many people with dilated cardiomyopathy have no symptoms. Some that do have only minor ones, and live a normal life. Others develop symptoms that may get worse as their heart gets sicker.
Symptoms of DCM can happen at any age and may include:
DCM can be inherited, but it’s usually caused by other things, including:
It can also happen in women after they give birth. That’s called postpartum cardiomyopathy.
Your doctor will decide if you have DCM after he looks at things like:
Another test that’s rarely done to find the cause of cardiomyopathy is called a myocardial biopsy, or heart biopsy. A tissue sample is taken from the heart and examined under a microscope.
If you have a relative with dilated cardiomyopathy, ask your doctor if you should be screened for it. Genetic testing may also be available to find abnormal genes.
In the case of dilated cardiomyopathy, it’s aimed at making the heart stronger and getting rid of substances in the bloodstream that enlarge the heart and lead to more severe symptoms:
Medications: To manage heart failure, most people take drugs, such as a:
If you have an arrhythmia(irregular heartbeat), your doctor may give you medicine to control your heart rate or make them happen less often. Blood thinners may also be used to prevent blood clots.
Lifestyle changes: If you have heart failure, you should have less sodium, based on your doctor’s recommendations. He may point you toward aerobic exercise, but don’t do heavy weightlifting.
People with severe DCM may need one of the following surgeries:
Cardiac resynchronization by biventricular pacemaker: For some people with DCM, stimulating the right and left ventricles with this helps your heart’s contractions get stronger. This improves your symptoms and lets you exercise more.
The pacemaker also will help people with heart block (a problem with the heart’s electrical system) or some bradycardias (slow heart rates).
Implantable cardioverter defibrillators (ICD): These are suggested for people at risk for life-threatening arrhythmias or sudden cardiac death. It constantly monitors your heart’s rhythm. When it finds a very fast, abnormal rhythm, it ”shocks” the heart muscle back into a healthy beat.
Surgery: Your doctor may recommend a surgery for coronary artery disease or valve disease. You may be eligible for one to fix your left ventricle or one that gives you a device to help your heart work better.
Heart transplant: These are usually just for those with end-stage heart failure. You’ll go through a selection process. Hearts that can be used are in short supply. Also, you must be both sick enough that you need a new heart, and healthy enough to have the procedure.