What is HIV? What is AIDS?
HIV (human immunodeficiency virus) is a virus that attacks the immune system, the body’s natural defense system. Without a strong immune system, the body has trouble fighting off disease. Both the virus and the infection it causes are called HIV.
White blood cells are an important part of the immune system. HIV infects and destroys certain white blood cells called CD4+ cells. If too many CD4+ cells are destroyed, the body can no longer defend itself against infection.
The last stage of HIV infection is AIDS (acquired immunodeficiency syndrome). People with AIDS have a low number of CD4+ cells and get infections or cancers that rarely occur in healthy people. These can be deadly.
But having HIV doesn’t mean you have AIDS. Even without treatment, it takes a long time for HIV to progress to AIDS-usually 10 to 12 years.
When HIV is diagnosed before it becomes AIDS, medicines can slow or stop the damage to the immune system. If AIDS does develop, medicines can often help the immune system return to a healthier state.
With treatment, many people with HIV are able to live long and active lives.
There are two types of HIV:
- HIV-1, which causes almost all the cases of AIDS worldwide
- HIV-2, which causes an AIDS-like illness. HIV-2 infection is uncommon in North America.

What causes HIV?
HIV infection is caused by the human immunodeficiency virus. You can get HIV from contact with infected blood, semen, or vaginal fluids.
- Most people get the virus by having unprotected sex with someone who has HIV.
- Another common way of getting it is by sharing drug needles with someone who is infected with HIV.
- The virus can also be passed from a mother to her baby during pregnancy, birth, or breastfeeding.
HIV doesn’t survive well outside the body. So it can’t be spread by casual contact like kissing or sharing drinking glasses with an infected person.
What are the symptoms?
HIV may not cause symptoms early on. People who do have symptoms may mistake them for the flu or mono. Common early symptoms include:
- Fever.
- Sore throat.
- Headache.
- Muscle aches and joint pain.
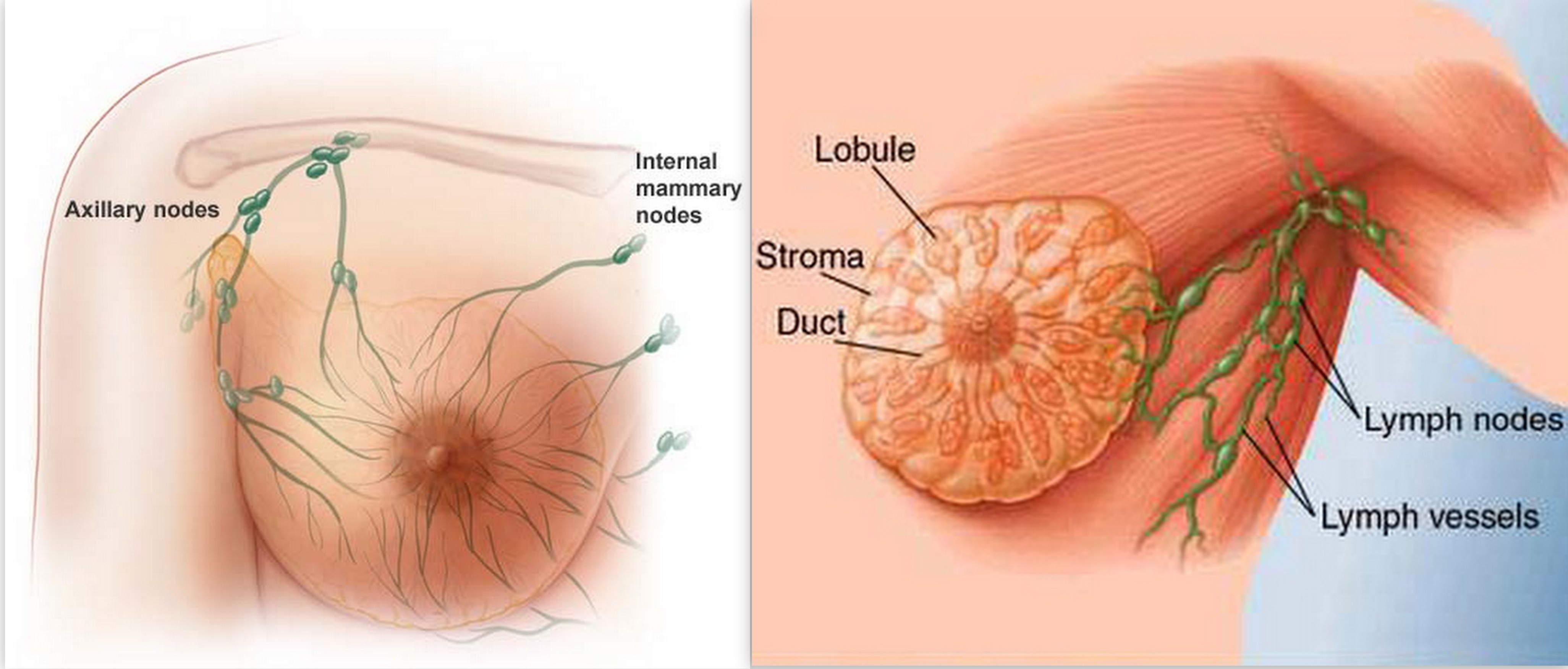
- Swollen glands (swollen lymph nodes).
- Skin rash.
Symptoms may appear from a few days to several weeks after a person is first infected. The early symptoms usually go away within 2 to 3 weeks.
After the early symptoms go away, an infected person may not have symptoms again for many years. After a certain point, symptoms reappear and then remain. These symptoms usually include:
- Swollen lymph nodes.
- Extreme tiredness.
- Weight loss.
- Fever.
- Night sweats.
How is HIV diagnosed?
A doctor may suspect HIV if symptoms last and no other cause can be found.
If you have been exposed to HIV, your immune system will make antibodiesto try to destroy the virus. Doctors use tests to find these antibodies in urine, saliva, or blood.
If a test on urine or saliva shows that you are infected with HIV, you will probably have a blood test to confirm the results.
Most doctors use two blood tests, called the ELISA and the Western blot. If the ELISA is positive (meaning that HIV antibodies are found), a Western blot or other test will be done to be sure.
HIV antibodies usually show up in the blood within 3 months but can take as long as 6 months. If you think you have been exposed to HIV but you test negative for it:
- Get tested again. Tests at 6, 12, and 24 weeks can be done to be sure you are not infected.
- Meanwhile, take steps to prevent the spread of the virus, in case you do have it.
You can get HIV testing in most doctors’ offices, public health clinics, hospitals, and Planned Parenthood clinics. You can also buy a home HIV test kit in a drugstore or by mail order. Make sure it’s one that is approved by the Food and Drug Administration (FDA). If a home test is positive, see a doctor to have the result confirmed and to find out what to do next.
If you have been exposed to HIV, your immune system will make antibodiesto try to destroy the virus. Doctors use tests to find these antibodies in urine, saliva, or blood.
If a test on urine or saliva shows that you are infected with HIV, you will probably have a blood test to confirm the results.
Most doctors use two blood tests, called the ELISA and the Western blot. If the ELISA is positive (meaning that HIV antibodies are found), a Western blot or other test will be done to be sure.
HIV antibodies usually show up in the blood within 3 months but can take as long as 6 months. If you think you have been exposed to HIV but you test negative for it:
- Get tested again. Tests at 6, 12, and 24 weeks can be done to be sure you are not infected.
- Meanwhile, take steps to prevent the spread of the virus, in case you do have it.
You can get HIV testing in most doctors’ offices, public health clinics, hospitals, and Planned Parenthood clinics. You can also buy a home HIV test kit in a drugstore or by mail order. Make sure it’s one that is approved by the Food and Drug Administration (FDA). If a home test is positive, see a doctor to have the result confirmed and to find out what to do next.
How is it treated?
The standard treatment for HIV is a combination of medicines called antiretroviral therapy, or ART. Antiretroviral medicines slow the rate at which the virus multiplies.
Taking these medicines can reduce the amount of virus in your body and help you stay healthy.
Medical experts recommend that people begin treatment for HIV as soon as they know that they are infected.1, 2
To monitor the HIV infection and its effect on your immune system, a doctor will regularly do two tests:
- Viral load, which shows the amount of virus in your blood.
- CD4+ cell count, which shows how well your immune system is working.
After you start treatment, it’s important to take your medicines exactly as directed by your doctor. When treatment doesn’t work, it is often because HIV has become resistant to the medicine. This can happen if you don’t take your medicines correctly.
How can you prevent HIV?
HIV is often spread by people who don’t know they have it. So it’s always important to protect yourself and others by taking these steps:
- Practice safer sex. Use a condom every time you have sex (including oral sex) until you are sure that you and your partner aren’t infected with HIV or other sexually transmitted infection (STI).
- Don’t have more than one sex partner at a time. The safest sex is with one partner who has sex only with you.
- Talk to your partner before you have sex the first time. Find out if he or she is at risk for HIV. Get tested together. Getting tested again at 6, 12, and 24 weeks after the first test can be done to be sure neither of you is infected. Use condoms in the meantime.
- Don’t drink a lot of alcohol or use illegal drugs before sex. You might let down your guard and not practice safer sex.
- Don’t share personal items, such as toothbrushes or razors.
- Never share needles or syringes with anyone.
If you are at high risk for getting infected with HIV, you can take antiretroviral medicine to help protect yourself from HIV infection. Experts may recommend this for:
- People whose sexual practices put them at high risk for HIV infection, such as men who have sex with men and people who have many sex partners.
- People who inject illegal drugs, especially if they share needles.
- Adults who have a sex partner with HIV.
To keep your risk low, you still need to practice safer sex even while you are taking the medicine.



























.jpg)