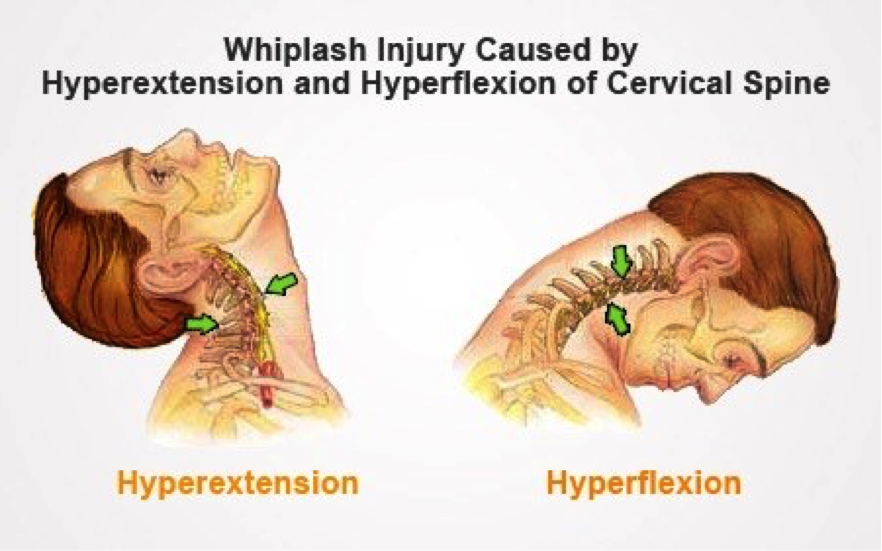
Neck strain is often just called whiplash. Although it’s usually associated with car accidents, any impact or blow that causes your head to jerk forward or backward can cause neck strain. The sudden force stretches and tears the muscles and tendons in your neck.
Neck strain afflicts many amateur and professional athletes. People who play contact sports like football are especially prone to neck strain.
Neck strains are often confused with neck sprains. They’re a bit different. Neck strains are caused by damage to the muscle or the tendons, bands of tissue that connect muscles to bones. Neck sprains are caused by tearing of the ligaments, the tissues that connect the bones to each other.
However, the differences between these strains and sprains probably won’t mean much to you. The causes, symptoms, and treatment of neck sprains and neck strains are usually the same.
What Are the Symptoms of Whiplash?
The pain of whiplash is often hard to ignore. The symptoms may include:
- Pain, decreased range of motion, and tightness in the neck. The muscles may feel hard or knotted.
- Pain when rocking your head from side to side or backward and forward.
- Pain or stiffness when moving your head to look over each shoulder.
- Tenderness.
- Headaches at the base of the skull that radiate towards the forehead.
Sometimes, the pain of a neck strain is immediate. In other cases, it can take several hours or days before your neck begins to hurt.
The blow that causes neck strain can sometimes cause a concussion, too. Since concussions can be serious, you need to see a doctor right away. You need emergency medical care if you have a headache that worsens or persists, have weakness or trouble talking, or are confused, dizzy, nauseous, excessively sleepy, or unconscious.
To diagnose neck strain, your doctor will give you a thorough examination. You may also need X-rays, CT (computed tomography) scans, and other tests, to rule out other problems.
Here’s the good news: given time, whiplash should heal on its own. To help with recovery, you should:
- Ice your neck to reduce pain and swelling as soon as you can after the injury. Do it for 15 minutes every 3-4 hours for 2-3 days. Wrap the ice in a thin towel or cloth to prevent injury to the skin.
- Take painkillers or other drugs, if recommended by your doctor. Non-steroidal anti-inflammatory drugs (NSAIDs), like ibuprofen (Advil, Motrin) or naproxen (Aleve), will help with pain and swelling. However, these medicines can have side effects. Never use them regularly unless your doctor specifically says you should. Check with your doctor before taking them if you take other medicines or have any medical problems. If over the counter medications do not work, prescription painkillers and muscle relaxants may be necessary.
- Use a neck brace or collar to add support, if your doctor recommends it. However, they are not recommended for long-term use, because they can actually weaken the muscles in your neck.
- Apply moist heat to your neck — but only after 2-3 days of icing it first. Use heat on your neck only after the initial swelling has gone down. You could use warm, wet towels or take a warm bath.
- Other treatments, like ultrasound and massage, may also help.