Tetralogy of Fallot is a rare condition caused by a combination of four heart defects that are present at birth (congenital).
These defects, which affect the structure of the heart, cause oxygen-poor blood to flow out of the heart and to the rest of the body. Infants and children with tetralogy of Fallot usually have blue-tinged skin because their blood doesn’t carry enough oxygen.
Tetralogy of Fallot is often diagnosed during infancy or soon after. However, tetralogy of Fallot might not be detected until later in life in some adults, depending on the severity of the defects and symptoms.
With early diagnosis followed by appropriate surgical treatment, most children and adults who have tetralogy of Fallot live relatively normal lives, though they’ll need regular medical care throughout life and might have restrictions on exercise.
Symptoms
Tetralogy of Fallot symptoms vary, depending on the extent of obstruction of blood flow out of the right ventricle and into the lungs. Signs and symptoms may include:
- A bluish coloration of the skin caused by blood low in oxygen (cyanosis)
- Shortness of breath and rapid breathing, especially during feeding or exercise
- Loss of consciousness (fainting)
- Clubbing of fingers and toes — an abnormal, rounded shape of the nail bed
- Poor weight gain
- Tiring easily during play or exercise
- Irritability
- Prolonged crying
- A heart murmur
Tet spells
Sometimes, babies who have tetralogy of Fallot will suddenly develop deep blue skin, nails and lips after crying or feeding, or when agitated.
These episodes are called tet spells and are caused by a rapid drop in the amount of oxygen in the blood. Tet spells are most common in young infants, around 2 to 4 months old. Toddlers or older children might instinctively squat when they’re short of breath. Squatting increases blood flow to the lungs.
When to see a doctor
Seek medical help if you notice that your baby has the following symptoms:
- Difficulty breathing
- Bluish discoloration of the skin
- Passing out or seizures
- Weakness
- Unusual irritability
If your baby becomes blue (cyanotic), place your baby on his or her side and pull your baby’s knees up to his or her chest. This helps increase blood flow to the lungs.
Causes
Tetralogy of Fallot occurs during fetal growth, when the baby’s heart is developing. While factors such as poor maternal nutrition, viral illness or genetic disorders might increase the risk of this condition, in most cases the cause of tetralogy of Fallot is unknown.
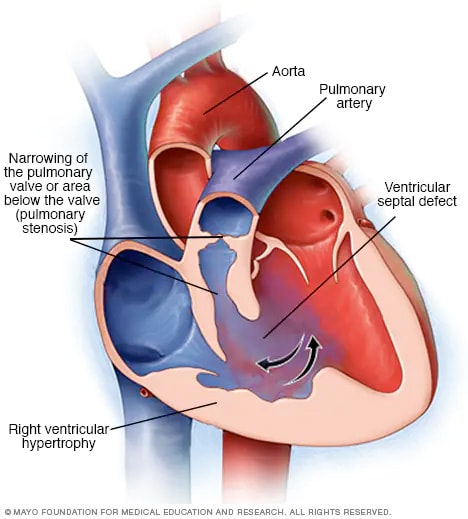
The four abnormalities that make up the tetralogy of Fallot include:
- Pulmonary valve stenosis. Pulmonary valve stenosis is a narrowing of the pulmonary valve — the valve that separates the lower right chamber of the heart (right ventricle) from the main blood vessel leading to the lungs (pulmonary artery).Narrowing (constriction) of the pulmonary valve reduces blood flow to the lungs. The narrowing might also affect the muscle beneath the pulmonary valve. In some severe cases, the pulmonary valve doesn’t form properly (pulmonary atresia) and causes reduced blood flow to the lungs.
- Ventricular septal defect. A ventricular septal defect is a hole (defect) in the wall (septum) that separates the two lower chambers of the heart — the left and right ventricles. The hole allows deoxygenated blood in the right ventricle — blood that has circulated through the body and is returning to the lungs to replenish its oxygen supply — to flow into the left ventricle and mix with oxygenated blood fresh from the lungs.Blood from the left ventricle also flows back to the right ventricle in an inefficient manner. This ability for blood to flow through the ventricular septal defect reduces the supply of oxygenated blood to the body and eventually can weaken the heart.
- Overriding aorta. Normally the aorta — the main artery leading out to the body — branches off the left ventricle. In tetralogy of Fallot, the aorta is shifted slightly to the right and lies directly above the ventricular septal defect.In this position the aorta receives blood from both the right and left ventricles, mixing the oxygen-poor blood from the right ventricle with the oxygen-rich blood from the left ventricle.
- Right ventricular hypertrophy. When the heart’s pumping action is overworked, it causes the muscular wall of the right ventricle to thicken. Over time this might cause the heart to stiffen, become weak and eventually fail.
Some children or adults who have tetralogy of Fallot may have other heart defects, such as a hole between the heart’s upper chambers (atrial septal defect), a right aortic arch or abnormalities of the coronary arteries.
Risk factors
While the exact cause of tetralogy of Fallot is unknown, various factors might increase the risk of a baby being born with this condition. These risk factors include:
- A viral illness during pregnancy, such as rubella (German measles)
- Alcoholism during pregnancy
- Poor nutrition during pregnancy
- A mother older than age 40
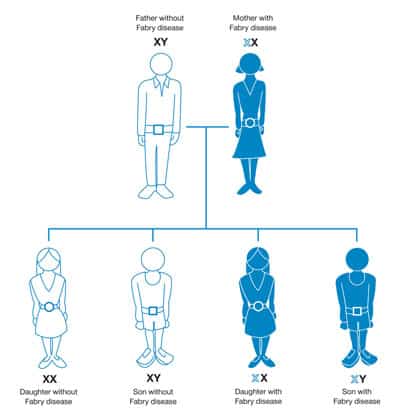
- A parent who has tetralogy of Fallot
- The presence of Down syndrome or DiGeorge syndrome
Complications
All babies who have tetralogy of Fallot need corrective surgery. Without treatment, your baby might not grow and develop properly.
Your baby may also be at an increased risk of serious complications, such as infective endocarditis — an infection of the inner lining of the heart or heart valve caused by a bacterial infection.
Untreated cases of tetralogy of Fallot usually develop severe complications over time, which might result in death or disability by early adulthood.
Treatment
Surgery is the only effective treatment for tetralogy of Fallot. Surgical options include intracardiac repair or a temporary procedure that uses a shunt. However, most babies and older children have intracardiac repair.
Your or your child’s doctors will determine the most appropriate surgery and the timing of the surgery based on your or your child’s condition.
In some cases your child may need medicine to keep the opening between two large blood vessels in the heart open. This can help to maintain blood flow from the heart to the lungs before intracardiac repair.
Intracardiac repair
This open-heart surgery is usually done during the first year after birth and involves several repairs. Adults with tetralogy of Fallot rarely may undergo this procedure if they didn’t have surgical repair as children.
The surgeon places a patch over the ventricular septal defect to close the hole between the lower chambers of the heart (ventricles).
He or she also repairs or replaces the narrowed pulmonary valve and widens the pulmonary arteries to increase blood flow to the lungs.
Because the right ventricle won’t need to work as hard to pump blood after this procedure, the right ventricle wall will go back to its normal thickness. After intracardiac repair, the oxygen level in the blood increases and symptoms will lessen.
Temporary surgery
Occasionally babies need to undergo a temporary (palliative) surgery before having intracardiac repair in order to improve blood flow to the lungs. This procedure may be done if your baby was born prematurely or has pulmonary arteries that are undeveloped (hypoplastic).
In this procedure, the surgeon creates a bypass (shunt) between a large artery that branches off from the aorta and the pulmonary artery.
When your baby is ready for intracardiac repair, the surgeon removes the shunt during the procedure for intracardiac repair.
After surgery
While most babies and adults do well after intracardiac repair, long-term complications are common. Complications may include:
- Chronic pulmonary regurgitation, in which blood leaks through the pulmonary valve back into the pumping chamber (right ventricle)
- Other heart valve problems, such as blood leaking back through the tricuspid valve
- Holes in the wall between the ventricles (ventricular septal defects) that may continue to leak after repair or may need re-repair
- Enlarged right ventricle or left ventricle that isn’t working properly
- Irregular heartbeats (arrhythmias)
- Coronary artery disease
- Aortic root dilation, in which the ascending aorta enlarges
- Sudden cardiac death
Complications can continue throughout childhood, adolescence and adulthood for people with tetralogy of Fallot. Most adults with repaired tetralogy of Fallot may require another procedure or intervention during their lifetimes. It’s very important to have regular follow-up with a cardiologist trained in caring for people with congenital heart disease (pediatric cardiologist or adult congenital cardiologist) who can evaluate you and determine the appropriate timing of another intervention or procedure.
Sometimes blood flow to the lungs may still be restricted after intracardiac repair. Infants, children or adults with these complications might require additional surgeries. More commonly, there is leakage through the repaired pulmonary valve. Most adults with repaired tetralogy of Fallot may have pulmonary valve leakage (regurgitation) and may need to have the pulmonary valve replaced during their lifetimes. Your cardiologist will determine the most appropriate timing for this procedure.
Arrhythmias are common after repair and may be treated with medications, a procedure to treat the arrhythmias (ablation) or a special pacemaker device that treats life-threatening heart rhythms (implantable cardioverter-defibrillator).
In addition, as with any surgery, there’s a risk of infection, unexpected bleeding or blood clots.
Ongoing care
After surgery you or your child will need lifelong care with a cardiologist trained in treating congenital heart disease (adult congenital cardiologist or pediatric cardiologist), including routine follow-up appointments to make sure that the initial operation or procedure was successful and to monitor for any new complications.
Your or your child’s doctor may conduct a physical examination and order tests in regular follow-up appointments to evaluate and monitor your or your child’s condition.
The doctor might also recommend that you or your child limit strenuous physical activity, particularly if there’s any pulmonary valve leakage or obstruction, or arrhythmias.
Sometimes, antibiotics are recommended during dental procedures to prevent infections that might cause endocarditis — an inflammation of the lining of the heart. Antibiotics are especially important for those who have had prior endocarditis, have artificial valves or have had repair with prosthetic material. Ask the doctor what’s right for you or your child.