Bariatric Surgery Procedures
Bariatric surgical procedures cause weight loss by restricting the amount of food the stomach can hold, causing malabsorption of nutrients, or by a combination of both gastric restriction and malabsorption. Bariatric procedures also often cause hormonal changes. Most weight loss surgeries today are performed using minimally invasive techniques (laparoscopic surgery).
The most common bariatric surgery procedures are gastric bypass, sleeve gastrectomy, adjustable gastric band, and biliopancreatic diversion with duodenal switch.
Procedures:
- Gastric Bypass
- Sleeve Gastrectomy
- Adjustable Gastric Band
- Biliopancreatic Diversion with Duodenal Switch (BPD/DS)
Gastric Bypass
The Roux-en-Y Gastric Bypass – often called gastric bypass – is considered the ‘gold standard’ of weight loss surgery
Sleeve Gastrectomy
The Laparoscopic Sleeve Gastrectomy – often called the sleeve – is performed by removing approximately 80 percent of the stomach. The remaining stomach is a tubular pouch that resembles a banana
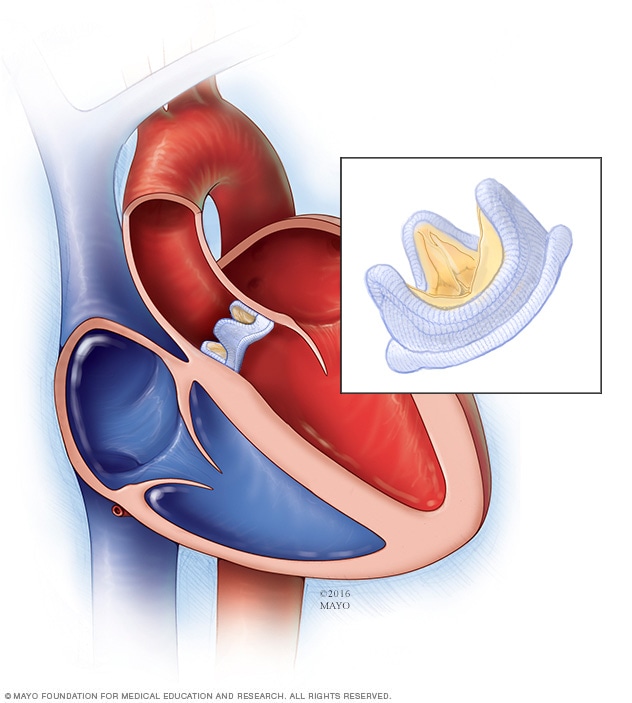
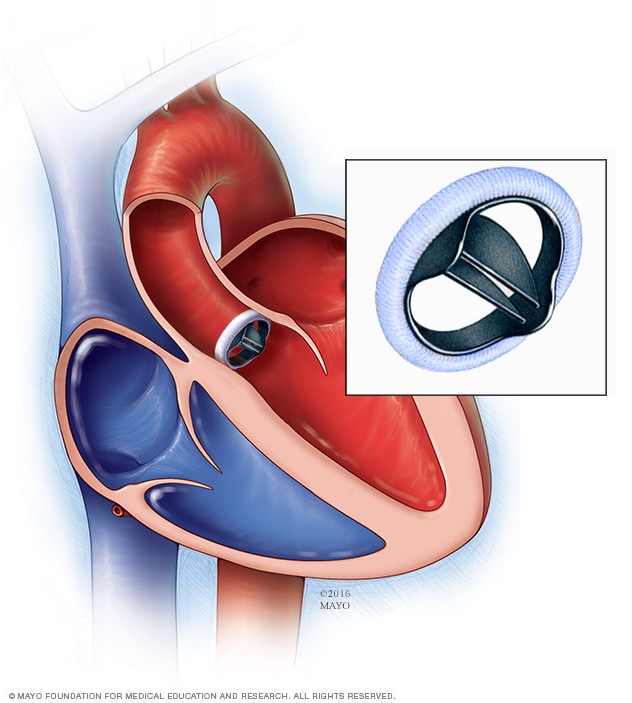
Adjustable Gastric Band
The Adjustable Gastric Band – often called the band – involves an inflatable band that is placed around the upper portion of the stomach, creating a small stomach pouch above the band, and the rest of the stomach below the band.
Biliopancreatic Diversion with Duodenal Switch (BPD/DS)
The Biliopancreatic Diversion with Duodenal Switch – abbreviated as BPD/DS – is a procedure with two components. First, a smaller, tubular stomach pouch is created by removing a portion of the stomach, very similar to the sleeve gastrectomy. Next, a large portion of the small intestine is bypassed.
The health benefits of bariatric surgery and the subsequent weight loss can be dramatic. Conditions such as diabetes, high blood pressure, asthma, heart disease, acid reflux, sleep apnea and gall bladder disease are just some of the health problems that can improve significantly or disappear all together. Other conditions that can be improved or eliminated include stress urinary incontinence, low back pain, and degenerative joint and disk disease. Life expectancy and the quality of life is dramatically improved with bariatric surgery and weight loss with the resolution of so many health problems experienced by the morbidly obese.
The advantage to bariatric surgery is the weight loss is typically much faster than diet and exercise alone. Bariatric surgery controls the food intake by reducing the amount of food able to be consumed and can also limit caloric absorption, depending on the surgical method chosen