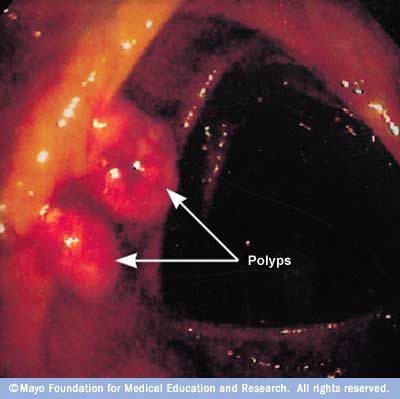
Colon polyp is a small clump of cells that forms on the lining of the colon. Most colon polyps are harmless. But over time, some colon polyps can develop into colon cancer, which is often fatal when found in its later stages.
There are two main categories of polyps, non-neoplastic and neoplastic. Non-neoplastic polyps include hyperplastic polyps, inflammatory polyps and hamartomatous polyps. These types of polyps typically do not become cancerous. Neoplastic polyps include adenomas and serrated types. In general, the larger a polyp, the greater the risk of cancer, especially with neoplastic polyps.
Anyone can develop colon polyps. You’re at higher risk if you’re 50 or older, are overweight or a smoker, or have a personal or family history of colon polyps or colon cancer.
Colon polyps often don’t cause symptoms. It’s important to have regular screening tests, such as a colonoscopy, because colon polyps found in the early stages can usually be removed safely and completely. The best prevention for colon cancer is regular screening for polyps.
Symptoms
Colon polyps often cause no symptoms. You might not know you have a polyp until your doctor finds it during an examination of your bowel.
But some people with colon polyps experience:
- Rectal bleeding. This can be a sign of colon polyps or cancer or other conditions, such as hemorrhoids or minor tears in your anus.
- Change in stool color. Blood can show up as red streaks in your stool or make stool appear black. A change in color may also be caused by foods, medications and supplements.
- Change in bowel habits. Constipation or diarrhea that lasts longer than a week may indicate the presence of a large colon polyp. But a number of other conditions can also cause changes in bowel habits.
- Pain. A large colon polyp can partially obstruct your bowel, leading to crampy abdominal pain.
- Iron deficiency anemia. Bleeding from polyps can occur slowly over time, without visible blood in your stool. Chronic bleeding robs your body of the iron needed to produce the substance that allows red blood cells to carry oxygen to your body (hemoglobin). The result is iron deficiency anemia, which can make you feel tired and short of breath.
When to see a doctor
See your doctor if you experience:
- Abdominal pain
- Blood in your stool
- A change in your bowel habits that lasts longer than a week
You should be screened regularly for polyps if:
- You’re age 50 or older.
- You have risk factors, such as a family history of colon cancer. Some high-risk individuals should begin regular screening much earlier than age 50.
Causes:
There are two main categories of polyps, non-neoplastic and neoplastic. Non-neoplastic polyps include hyperplastic polyps, inflammatory polyps and hamartomatous polyps. Non-neoplastic polyps typically do not become cancerous.
Inflammatory polyps may be seen with ulcerative colitis or Crohn’s disease of the colon. Although the polyps themselves are not a significant threat, having ulcerative colitis or Crohn’s disease of the colon increases your overall risk of colon cancer.
Neoplastic polyps include adenomas and serrated types. Most colon polyps are adenomas. Serrated polyps may become cancerous, depending on their size and location in the colon. In general, the larger a polyp, the greater the risk of cancer, especially with neoplastic polyps.
-
Small polyps

- Large polyp

- Colon cancer
Treatment
Your doctor is likely to remove all polyps discovered during a bowel examination. The options for removal include:
- Removal with forceps or a wire loop (polypectomy). If a polyp is larger than 0.4 inches (about 1 centimeter), a liquid may be injected under it to lift and isolate the polyp from surrounding tissue so that it can be removed.
- Minimally invasive surgery. Polyps that are too large or that can’t be removed safely during screening are usually removed laparoscopically, which is performed by inserting an instrument called a laparoscope into the bowel.
- Colon and rectum removal. If you have a rare inherited syndrome, such as FAP, you may need surgery to remove your colon and rectum (total proctocolectomy).
Some types of colon polyp are far likelier to become malignant than are others. But a doctor who specializes in analyzing tissue samples (pathologist) usually must examine polyp tissue under a microscope to determine whether it’s potentially cancerous.
Follow-up care
If you have had an adenomatous polyp or a serrated polyp, you are at increased risk of colon cancer. The level of risk depends on the size, number and characteristics of the adenomatous polyps that were removed.
You’ll need follow-up screenings for polyps. Your doctor is likely to recommend a colonoscopy:
- In five to 10 years if you had only one or two small adenomas
- In three years if you had more than two adenomas, adenomas measuring 0.4 inches (about 1 centimeter) or larger, or certain adenomas
- Within three years if you had more than 10 adenomas
- Within six months if you had a very large adenoma or an adenoma that had to be removed in pieces
It’s important to fully prepare your colon before a colonoscopy. If stool remains in the colon and obstructs your doctor’s view of the colon wall, you will likely need a follow-up colonoscopy sooner than the guidelines specify.
Risk factors
Factors that may contribute to the formation of colon polyps or cancer include:
- Age. Most people with colon polyps are 50 or older.
- Inflammatory intestinal conditions, such as ulcerative colitis and Crohn’s disease.
- Family history. You’re more likely to develop colon polyps or cancer if you have a parent, sibling or child with them. If many family members have them, your risk is even greater. In some people, this connection isn’t hereditary.
- Tobacco and alcohol use.
- Obesity and lack of exercise.
- Race. African-Americans are at higher risk of developing colon cancer.
- Type 2 diabetes that isn’t well-controlled.
Hereditary polyp disorders
Rarely, people inherit genetic mutations that cause colon polyps to form. If you have one of these genetic mutations, you are at much higher risk of developing colorectal cancer. Screening and early detection can help prevent the development or spread of these cancers.
Hereditary disorders that cause colon polyps include:
- Lynch syndrome, also called hereditary nonpolyposis colorectal cancer. People with Lynch syndrome tend to develop relatively few colon polyps, but those polyps can quickly become malignant. Lynch syndrome is the most common form of inherited colon cancer and is also associated with tumors in the breast, stomach, small intestine, urinary tract and ovaries.
- Familial adenomatous polyposis (FAP), a rare disorder that causes hundreds or even thousands of polyps to develop in the lining of your colon beginning during your teenage years. If the polyps aren’t treated, your risk of developing colon cancer is nearly 100 percent, usually before age 40. Genetic testing can help determine your risk of FAP.
- Gardner’s syndrome, a variant of FAP that causes polyps to develop throughout your colon and small intestine. You may also develop noncancerous tumors in other parts of your body, including your skin, bones and abdomen.
- MYH-associated polyposis (MAP), a condition similar to FAP that is caused by mutations in the MYH gene. People with MAP often develop multiple adenomatous polyps and colon cancer at a young age. Genetic testing can help determine your risk of MAP.
- Peutz-Jeghers syndrome, a condition that usually begins with freckles developing all over the body, including the lips, gums and feet. Then noncancerous polyps develop throughout the intestines. These polyps may become malignant, so people with this condition have an increased risk of colon cancer.
- Serrated polyposis syndrome, a condition that leads to multiple serrated adenomatous polyps in the upper part of the colon. These polyps may become malignant.
Complications
Some colon polyps may become cancerous. The earlier polyps are removed, the less likely it is that they will become malignant.
Prevention
You can greatly reduce your risk of colon polyps and colorectal cancer by having regular screenings. Certain lifestyle changes also can help:
- Adopt healthy habits. Include plenty of fruits, vegetables and whole grains in your diet and reduce your fat intake. Limit alcohol consumption and quit tobacco. Stay physically active and maintain a healthy body weight.
- Talk to your doctor about calcium and vitamin D. Studies have shown that increasing your consumption of calcium may help prevent recurrence of colon adenomas. But it isn’t clear whether calcium has any protective benefits against colon cancer. Other studies have shown that vitamin D may have a protective effect against colorectal cancer.
- Consider your options if you’re at high risk. If you have a family history of colon polyps, consider having genetic counseling. If you’ve been diagnosed with a hereditary disorder that causes colon polyps, you’ll need regular colonoscopies starting in young adulthood.

Post a comment