What is an aneurysm?
An aneurysm is an arterial condition in which the wall of an artery weakens, creating a bulge, or distension of the artery.
 A comparison between an artery with an aneurysm and two different types of artery. Note the cross-section showing a thinner artery wall in the third diagram for aneurysm, compared with normal and narrowed arteries.
A comparison between an artery with an aneurysm and two different types of artery. Note the cross-section showing a thinner artery wall in the third diagram for aneurysm, compared with normal and narrowed arteries.An aneurysm can occur in important arteries such as those supplying blood to the brain, and the aorta; the large artery that originates at the left ventricle of the heart and passes down through the chest and abdominal cavities.
The normal diameter of the aorta is around 0.8 inches. This width can bulge to beyond 2 inches with an aneurysm, a width that would typically necessitate surgical treatment.
An aneurysm can also occur in peripheral arteries – usually behind the knee (popliteal aneurysms) – although rupture of these is relatively uncommon.
The two most important common locations for aneurysms are:
- In the artery directly leaving the heart – an aortic aneurysm (including thoracic and, further down, abdominal aortic aneurysms)
- In an artery in the brain – a cerebral aneurysm.
Thoracic aortic aneurysm is often abbreviated to TAA, and abdominal aortic aneurysm to AAA. Brain aneurysms are often termed intracranial aneurysms, as well as “berry aneurysms” on account of their size and shape.
Two other examples of aneurysm are mesenteric artery aneurysm (affecting the artery supplying the intestines of the gut) and splenic artery aneurysm (occurring in the spleen, an abdominal organ).
Symptoms of aneurysm:
Most aneurysms do not themselves cause any symptoms.
Even if an aneurysm does not rupture, however, a large aneurysm may obstruct circulation to other tissues. An aneurysm can also contribute to the formation of blood clots that then obstruct smaller blood vessels, potentially causing ischemic stroke or other serious problems; this is known as thromboembolism.
Back pain can be a symptom of an aneurysm although most aneurysms are asymptomatic.
Abdominal aneurysms are sometimes associated with symptoms if they grow rapidly. Some people report abdominal or lower back pain, or a pulsating sensation in the abdomen.
Similarly, thoracic aneurysms can cause symptoms by affecting nearby tissues, including nerves and other blood vessels.
If an aneurysm compresses the laryngeal or vagus nerve, it can cause chest or back pain and symptoms such as coughing, wheezing and difficulty swallowing. Compression of the coronary artery can also cause chest pain.
Otherwise, aneurysms tend to produce symptoms only when there are complications such as rupture.
Symptoms can also be related to the cause of the aneurysm rather than the aneurysm itself. In the case of infection or vasculitis (blood vessel inflammation), for example, there may be fever, malaise or weight loss.
Complications of aneurysm
If an aneurysm has remained undetected, the first sign of it could be when there is a complication – in particular, a rupture – with symptoms resulting from this rather than the aneurysm itself.
The majority of people living with an aneurysm do not suffer any of the complications in the following list. Managing the risk factors is important, however, because all of these possibilities are serious.
Complications of aneurysm include:
 Brain aneurysm can lead to subarachnoid hemorrhage; a symptom of this stroke bleed is a sudden extreme headache.
Brain aneurysm can lead to subarachnoid hemorrhage; a symptom of this stroke bleed is a sudden extreme headache.
- Thromboembolism – depending on where the clot has traveled to, thromboembolism can cause pain in the extremities or the abdomen. If a clot travels to the brain, it can cause a stroke
- Dissection of the aorta – see below for more detail
- Severe chest and/or back pain – if a silent or diagnosed aortic aneurysm in the chest ruptures, severe chest or back pain may arise. Such symptoms may help hospital medical staff diagnose an aneurysm.
- Angina – certain types of aneurysm can lead to angina, another type of chest pain; the pain is related to narrowed arteries supplying the heart itself (causing myocardial ischemia and possibly heart attack).
- Sudden extreme headache – if a brain aneurysm leads to subarachnoid hemorrhage (a kind of stroke), the main symptom is sudden extreme headache; often so severe that it is unlike any previous experience of head pain.
- Other symptoms – with any aneurysm rupture there may be pain, low blood pressure, a rapid heart rate, and light-headedness.
Again, most people with an aneurysm will not suffer any of these complications, and the risk can be reduced by taking preventive steps.
Treatments for aneurysm
Not all cases of unruptured aneurysm need active treatment, but when an aneurysm ruptures, emergency surgery is needed.
More details follow for the treatment options against the two main types of aneurysm.
Aortic aneurysm treatment options
An aortic aneurysm, whether abdominal or thoracic, may not need any active treatment and instead may just be monitored regularly. Medications and preventive measures may form part of conservative management or they may accompany active surgical treatment – through open or endovascular surgery.
Aortic aneurysm surgery can be performed as open surgery or as endovascular surgery.
Aneurysms that rupture require emergency surgery. Without immediate repair, a ruptured aneurysm is always fatal in the thoracic aorta, and almost always fatal in the abdominal aorta.
The decision to operate on an unruptured aneurysm in the aorta depends on a number of factors related to the individual patient, as well as to features of the aneurysm itself:
- Individual factors – age, general health, coexisting conditions and personal choice
- The aneurysm’s characteristics – size relative to location in the thorax or abdomen and the rate of growth
- Other factors – chronic abdominal pain or risk of thromboembolism may make surgery a good option.
An aortic aneurysm that has a larger diameter (about 2 inches or 5 cm) is more likely to prompt a recommendation of surgery, as is an aneurysm which is growing more quickly (a little less than 1/4 inch over the last 6-12 months).
For both elective unruptured and emergency ruptured cases, surgery can take one of two forms:
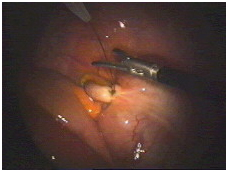
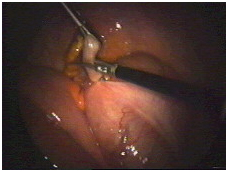
- Open surgery to fit a synthetic or stent graft
- Endovascular stent-graft surgery.
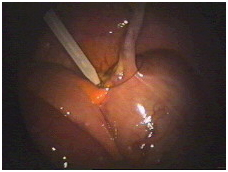
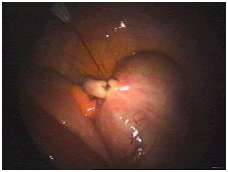
Endovascular surgery involves accessing the blood vessels through a small incision near the hip. In stent-graft surgery, an endovascular graft is inserted through this incision using a catheter and is positioned in the aorta to seal off the aneurysm.
In the emergency of a ruptured abdominal aortic aneurysm, the decision over which procedure to perform will be urgent. For elective operations to repair unruptured aneurysms, a review published in 2014 sought to determine the relative risks and benefits of open vs. endovascular surgery.
The review found that while there was a lack of robust studies comparing the two options directly, similar rates of complication were reported for both types of surgery.
The evidence suggested that endovascular aneurysm repair (EVAR) was “less invasive,” but the procedure did “not always significantly alter the postoperative course or length of hospital stay for patients.”
The authors concluded that open surgery still had a role for those patients who were not suitable for endovascular surgery.
Endovascular surgery has become the generally preferred method of aortic aneurysm surgery because of:
- Shorter operative times
- Often shorter hospital stays
- Better levels of surgical experience
- A perceived lower risk of disease or death surrounding surgery compared with laparoscopic surgery (although the review found this could be more perception than reality).
Endovascular surgery for the repair of aortic aneurysms does carry the following risks however, in addition to the usual risks of surgery:
- Bleeding around the graft (which requires additional surgery)
- Bleeding before or after the procedure
- Blockage of the stent
- Nerve damage, resulting in weakness, pain or numbness in the leg
- Kidney failure
- Reduced blood supply to the legs, kidneys or other organs
- Erectile dysfunction
- Unsuccessful surgery that then requires open surgery
- Slippage of the stent.
Cerebral aneurysm treatment options
Surgical treatment of an aneurysm in the brain is reserved for cases that present a high risk of rupture.
Aneurysms that are less likely to burst are not treated surgically because of the potential risk of brain-damage resulting from possible surgical complications.
In lieu of surgery, patients are given guidance on how to monitor and modify, where possible, the risk factors for rupture of a brain aneurysm. This will likely involve monitoring blood pressure – see prevention below.
Where a ruptured brain aneurysm has led to a subarachnoid hemorrhage (a medical emergency), a patient may be admitted to hospital and undergo brain surgery.
Such a procedure would aim to close off the artery that ruptured due to the aneurysm, in the hope of preventing another bleed.
Prevention of aneurysm
The single most important way a person can reduce their risk of developing an aneurysm is to not smoke or to quit if already smoking. Smoking is not only the strongest risk factor for the development of an aortic aneurysm, it is also one of the greatest risk factors for an aneurysm growing and rupturing.
Smoking is the strongest risk factor for both the development and rupture of aneurysms.
Smoking is a greater risk factor for aneurysm than it is for atherosclerosis, the cardiovascular disease where fatty deposits accumulate on the arterial wall and which can weaken artery walls.
The fact that smoking is also a big risk factor for atherosclerosis is directly relevant, however, because most aneurysms are caused by weakening of the artery wall brought on by atherosclerosis:
Studies have shown that continued smoking induces a significantly faster expansion of aortic aneurysms – by about 0.4 millimeters a year).
Brain aneurysms are not always possible to avoid to the same extent as aortic aneurysms because ruptured brain aneurysms causing subarachnoid hemorrhage stroke can be congenital – present at birth.
Brain aneurysm has both genetic and environmental risk factors, and a history of brain aneurysms in the family is an established risk factor, as is increasing age. However, known risk factors also include, alongside hypertension (high blood pressure), smoking.
Cigarette smoke is also a major source of free radicals which cause oxidative stress. Oxidative stress and resulting tissue damage can occur due to higher production or reduced removal of free radicals. Oxidative stress can also increase inflammation, which contributes to the formation and rupture of cerebral aneurysms.