Dysentery is an intestinal inflammation, especially in the colon, that can lead to severe diarrhea with mucus or blood in the feces.
Patients typically experience mild to severe abdominal pain or stomach cramps. In some cases, untreated dysentery can be life-threatening, especially if the infected person cannot replace lost fluids fast enough.
There are two main types of dysentery:
- Bacillary dysentery, caused by Shigella, a bacterium.
- Amoebic dysentery (amoebiasis) This is caused by Entamoeba histolytica, a type of amoeba. An amoeba is a protozoan (single-celled) organism that constantly changes shape.
Causes of dysentery :
Dysentery is mainly caused by a bacterial or protozoan (one cell organism, such as an amoeba) infection. It can also be caused by a parasitic worm infestation. More rarely, a chemical irritant or viral infection can also be a cause.
Causes of bacillary dysentery:
An infection with a bacillus of the Shigella group is the most common type of dysentery. According to the National Health Service (NHS), UK, Shigella sonnei is the most common, followed by Shigella flexneri, Shigella boydii and Shigella dysenteriae, the last one listed produces the most severe symptoms.
Poor hygiene is the main cause of bacillary dysentery infection. However, it can also spread because of tainted food.
Causes of amoebic dysentery
Amoebic dysentery is usually caused by infection with the Entamoeba histolytica amoeba.
Amoebic dysentery is more common in the tropics while bacillary dysentery is more common elsewhere.
The amoeba group together and form a cyst, the cysts come out of the body in human feces. In areas of poor sanitation, these cysts (which can survive for a long time), can contaminate food and water, and infect other humans. The cysts can also linger in infected people’s hands after going to the toilet. Good hygiene practice reduces the risk of infecting other people.
Symptoms of dysentery:
A symptom is something the patient feels and reports, while a sign is something other people, such as the doctor notice. For example, pain may be a symptom while a rash may be a sign.
Abdominal pain, diarrhea and fatigue are possible symptoms of dysentery.
In developed countries signs and symptoms of dysentery tend to be much milder than in developing nations or tropical areas. Patients with mild symptoms will have a slight stomach ache (cramping), and will frequently go to the toilet because of diarrhea.
Symptoms usually appear from one to three days after the person has become infected – this is called the incubation period. In most cases the patient recovers completely within a week. How often the individual goes to the toilet and has mucus or blood in feces usually depend on what is causing the disease.
In some cases people who get dysentery also develop lactose intolerance, which can take a long time to go away, sometimes even years.
Symptoms of amoebic dysentery include:
- abdominal pain
- fever and chills
- nausea and vomiting
- watery diarrhea, which can contain blood, mucus or pus
- painful passing of stools
- fatigue
- intermittent constipation.
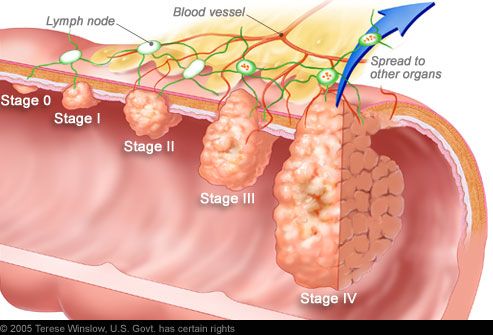
The amoeba can tunnel through the intestinal wall and spread into the bloodstream and infect other organs; ulcers can develop, these ulcers may bleed, causing blood in stools.
In some cases symptoms may persist for several weeks, but usually only last a few days. The amoebas may continue living within the host (the human) even after symptoms have gone, increasing the likelihood of a recurrence when the person’s defenses are down. The amoebas are less likely to survive if the patient receives treatment.
Signs and symptoms of bacillary dysentery – as in other types, symptoms tend to appear from one to three days after the person has been infected. Most typically, there is just mild stomachache and diarrhea, and no blood or mucus in the feces. For many, symptoms are so mild they do not even bother going to the doctor, and the problem resolves in a few days. Initially, the infected person goes to the toilet frequently with diarrhea.
Although much less common, some people with bacillary dysentery may have blood or mucus in their feces, abdominal pain may be intense, there may be an elevated body temperature (fever), nausea and vomiting.
Treatments for dysentery:
Rehydration therapy – initially this is done using oral rehydration; the patient is encouraged to drink plenty of liquids. Diarrhea, as well as vomiting results in loss of fluids that have to be replaced to prevent dehydration. If the diarrhea and/or vomiting is profuse the medical team may recommend intravenous fluid replacement – the patient will be on a drip.
Antibiotics and amoebicidal drugs – experts say that if possible, the administration of medications to kill the cause of the dysentery should be held back until lab tests determine whether the illness is being caused by a bacterium or amoeba. If this is not possible, depending on the severity of symptoms, the patient may be given a combinations of antibiotic and amoebicidal medication.
If symptoms are not severe and the doctor determines it is Bacillary dysentery (Shigella), the patient most likely will receive no medication – in the vast majority of cases the illness will resolve within a week. Oral rehydration is important.
If amoebic dysentery is diagnosed the patient will probably start with a 10-day course of an antimicrobial medication, such as Flagyl (metronidazole). Diloxanide furoate, paromomycin (Humatin), or iodoquinol (Yodoxin) may also be prescribed to make sure the amoeba does not survive inside the body after symptoms have gone.
Antirheumatic drug Ridaura (auranofin) may offer a cheap, low-dose treatment for the amoebic infections that cause dysentery in humans globally.