By the time you sign up for back surgery, your doctor will probably have tried a number of treatments to ease your back pain. While there are no guarantees the operation will provide relief, there are lots of options. Learn as much as you can about back surgery ahead of time. The more you know, the better the choice you’ll make.
What Are the Benefits?
Often, the result is more than just a drop in pain. You may find:
- You can move around better.
- You’re more physically fit.
- Your mood improves.
- You don’t need to take as much pain medicine.
- You can go back to work.
- You’re more productive at work
Risks:
That said, any operation will have some degree of risk, including:
- Reaction to anesthesia or other drugs
- Bleeding
- Infection
- Blood clots, for instance in your legs or lungs
- Heart attack
- Stroke
- Herniated disk
- Nerve damage, which can lead to weakness, paralysis, pain, sexual dysfunction, or loss of bowel or bladder control
The odds that something could go wrong go up for people with certain health conditions. They also vary by type of surgery. Part of your surgeon’s job is to identify potential problems. So talk it over before you head to the OR.
Each type comes with its own risks and benefits.
Spinal fusion. This is the most common surgery for back pain. The doctor will join spinal bones, called vertebrae, together. This limits the motion between them and how far your nerves can stretch. But it probably won’t limit your activity. It’s rare, but the bones don’t always fuse completely. Smoking can make this more likely. If it happens, you may need another operation to fix it.
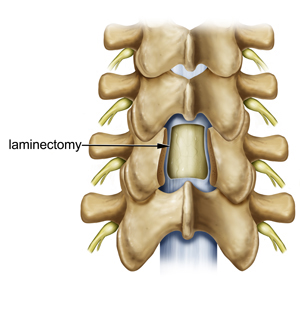
Laminectomy. In this procedure, a surgeon removes parts of the bone, bone spurs, or ligaments in your back. This relieves pressure on spinal nerves and can ease pain or weakness. It can make your spine less stable. If that happens, you’ll probably need a spinal fusion. Doctors sometimes do the two procedures together.
Foraminotomy. The surgeon cuts away bone at the sides of your vertebrae to widen the space where nerves exit your spine. The extra room may relieve pressure on the nerves and ease your pain. Like a laminectomy, this procedure can also make your spine less stable. So the surgeon may do a spinal fusion at the same time. That’ll increase the amount of time you need for recovery.
Diskectomy. Sometimes a disk, the cushion that separates your vertebrae, can slip out of place, press on a spinal nerve, and cause back pain. In a diskectomy, the surgeon removes all or part of the disk. He may have to make a big cut in your back, or he may be able to do it through a small one. Sometimes it’s part of a larger surgery that includes laminectomy, foraminotomy, or spinal fusion.
Disk replacement. A surgeon removes the damaged spinal disk and inserts an artificial one between your vertebrae. Unlike fusion, this lets you continue to move your spine. Recovery time may be shorter than for a spinal fusion, too. But there is a slight chance the new disk could slip or fall out of place and require repair.
Interlaminar implant. The surgeon implants a U-shaped device between two vertebrae in your lower back. It helps keep the space between them open and eases pressure on your spinal nerves. It can be done at the same time as a laminectomy. Unlike spinal fusion, the implant provides stability and lets you move your back almost like normal. You may not be able to bend backward as easily in that area.