Hypogonadism occurs when your sex glands produce little or no sex hormones. The sex glands, also called gonads, are primarily the testes in men and the ovaries in women. Sex hormones help control secondary sex characteristics, such as breast development in women, testicular development in men, and pubic hair growth. Sex hormones also play a role in the menstrual cycle and sperm production.
Hypogonadism may also be known as gonad deficiency. It may be called low serum testosterone or andropause when it happens in males.
Most cases of this disorder respond well to appropriate medical treatment.

There two types of hypogonadism are primary and central hypogonadism.
Primary Hypogonadism
Primary hypogonadism means that you don’t have enough sex hormones in your body due to a problem in your gonads. Your gonads are still receiving the message to produce hormones from your brain, but they aren’t able to produce them.
Central Hypogonadism (Secondary Hypogonadism)
In central hypogonadism, the problem lies in your brain. The hypothalamus and pituitary gland in your brain, which control your gonads, aren’t working properly.
The causes of primary hypogonadism include:
- autoimmune disorders, such as Addison’s disease and hypoparathyroidism
- genetic disorders, such as Turner syndrome and Klinefelter syndrome
- severe infections
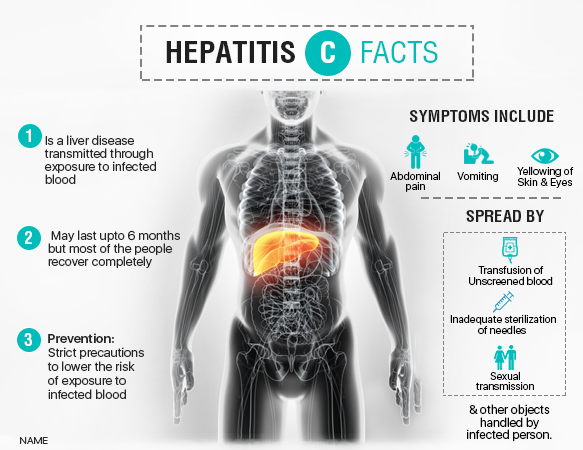
- liver and kidney diseases
- undescended testes
- hemochromatosis, which happens when your body absorbs too much iron
- radiation exposure
- surgery on your sex organs
Central, or secondary, hypogonadism may be due to:
- genetic disorders, such as Kallmann syndrome (abnormal hypothalamic development)
- infections, including HIV and AIDS
- pituitary disorders
- inflammatory diseases, including sarcoidosis, tuberculosis, and histiocytosis
- obesity
- rapid weight loss
- nutritional deficiencies
- use of steroids or opiates (especially long-term usage)
- brain surgery
- radiation exposure
- injury to your pituitary gland or hypothalamus
- a tumor in or near your pituitary gland
Symptoms that may affect females include:
- lack of menstruation
- slow or absent breast growth
- hot flashes
- loss of body hair
- low or absent sex drive
- milky discharge from your breasts
Symptoms that may affect males include:
- loss of body hair
- muscle loss
- abnormal breast growth
- reduced growth of penis and testicles
- erectile dysfunction
- osteoporosis
- low or absent sex drive
- infertility
- fatigue
- hot flashes
- difficulty concentrating
Your doctor will conduct a physical exam to confirm that your sexual development is at the proper level for your age. They may examine your muscle mass, body hair, and your sexual organs.
Hormone Tests
If your doctor thinks you might have hypogonadism, the first round of testing will involve checking your sex hormone levels. You’ll need a blood test to check your level of follicle-stimulating hormone (FSH) and luteinizing hormone (LH). Your pituitary gland makes these reproductive hormones.
You’ll have your estrogen level tested if you’re female. You’ll have your testosterone level tested if you’re male. These tests are usually drawn in the morning, which is when your hormone levels are highest. If you’re male, your doctor may also order a semen analysis to check your sperm count. Hypogonadism can reduce your sperm count.
Your doctor may order more blood tests to help confirm the diagnosis of hypogonadism and rule out any underlying causes.
Iron levels can affect your sex hormones. For this reason, your doctor may test for anemia, or iron deficiency. Your doctor may also wish to measure your prolactin levels. Prolactin is a hormone that promotes breast development and breast milk production in women, but it’s present in both genders. Your doctor may also check your thyroid hormone levels because thyroid problems can cause symptoms similar to hypogonadism.
Imaging Tests
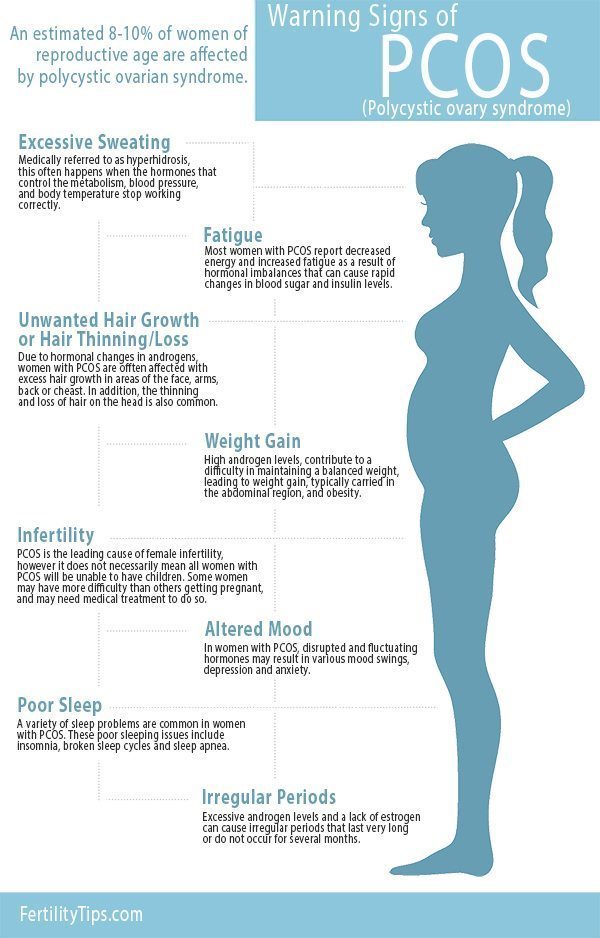
Imaging tests can also be useful in diagnosis. An ultrasound of the ovaries uses sound waves to create an image of the ovaries and check for any problems, including ovarian cysts and polycystic ovarian syndrome (PCOS). Your doctor may order MRI scans or CT scans to check for tumors in your pituitary gland.
Treatment for Hypogonadism in Women
Your treatment will involve increasing the amount of female sex hormones in your body if you’re a woman.
Your first line of treatment will probably be estrogen therapy if you’ve had a hysterectomy. Either a patch or pill can administer the supplemental estrogen hormone.
Because increased estrogen levels can increase your risk of endometrial cancer, you’ll be given a combination of estrogen and progesterone if women who haven’t had a hysterectomy. Progesterone can lower your risk of endometrial cancer if you’re taking estrogen.
Other treatments can target specific symptoms. If you’re a woman and you have a decreased sex drive, you may receive low doses of testosterone. If you have menstrual irregularities or trouble conceiving, you may receive injections of the hormone human choriogonadotropin (hCG) or pills containing FSH to trigger ovulation.
Treatment for Hypogonadism in Men
Testosterone is a male sex hormone. Testosterone replacement therapy (TRT) is a widely used treatment for hypogonadism in males. You can get testosterone replacement therapy by:
- injection
- patch
- gel
- lozenge
Injections of a gonadotropin-releasing hormone may trigger puberty or increase your sperm production.
Treatment for Hypogonadism in Men and Women
Treatment for males and females is similar if the hypogonadism is due to a tumor on the pituitary gland. Treatment may include radiation, medication, or surgery to shrink or remove the tumor.
Hypogonadism is a chronic condition that requires lifelong treatment. Your sex hormone level will probably decrease if you stop treatment.
Seeking support through therapy or support groups can help you before, during, and after treatment.