There are no specific medications to fix aortic valve stenosis. This is because the condition is irreversible once it occurs. Instead, your doctor can prescribe medication to treat the problems caused by the condition, or for the health issues that produced the condition in the first place. Surgery may be able to repair or replace the valve.
Although medication can’t cure aortic valve stenosis, your doctor may prescribe drugs to manage symptoms or reduce the burden on your heart. Some medications include:
Surgery options include:
Aortic valve repair
Surgeons rarely repair an aortic valve to treat aortic valve stenosis, and generally aortic valve stenosis requires aortic valve replacement. To repair an aortic valve, surgeons may separate valve flaps (cusps) that have fused.
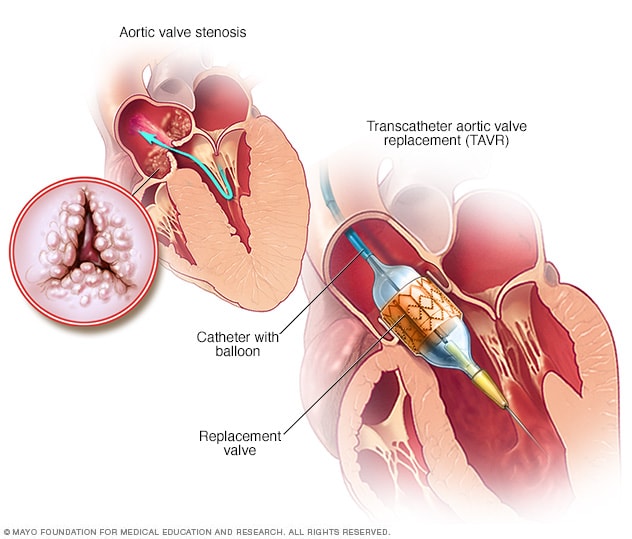
Balloon valvuloplasty
Doctors may conduct a procedure using a long, thin tube (catheter) to repair a valve with a narrowed opening (aortic valve stenosis). In this procedure, called balloon valvuloplasty, a doctor inserts a catheter with a balloon on the tip into an artery in your arm or groin and guides it to the aortic valve. The doctor performing the procedure then inflates the balloon, which expands the opening of the valve. The balloon is then deflated, and the catheter and balloon are removed.
The procedure can treat aortic valve stenosis in infants and children. However, the valve tends to narrow again in adults who’ve had the procedure, so it’s usually only performed in adults who are too ill for surgery or who are waiting for a valve replacement, as they typically need additional procedures to treat the narrowed valve over time.
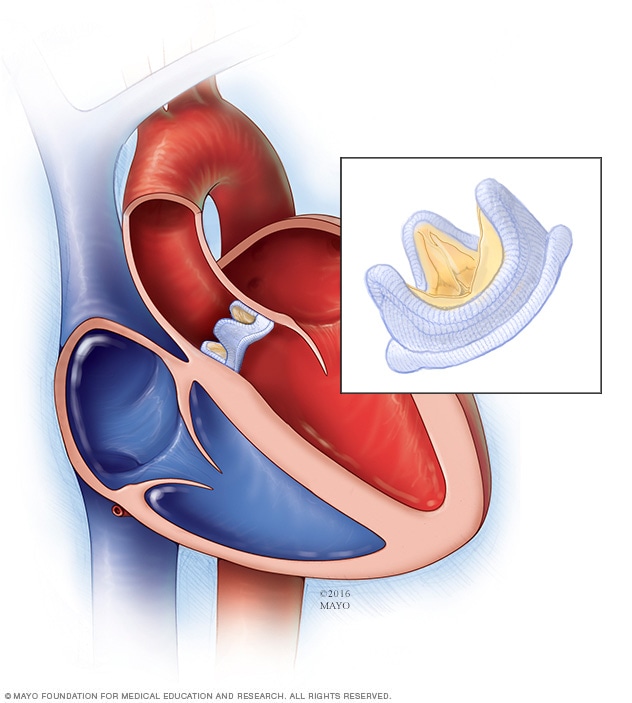
Aortic valve replacement
Aortic valve replacement is often needed to treat aortic valve stenosis. In aortic valve replacement, your surgeon removes the damaged valve and replaces it with a mechanical valve or a valve made from cow, pig or human heart tissue (biological tissue valve).
Biological tissue valves degenerate over time and may eventually need to be replaced. People with mechanical valves will need to take blood-thinning medications for life to prevent blood clots. Your doctor will discuss with you the benefits and risks of each type of valve and discuss which valve may be appropriate for you.
Doctors may perform a less invasive procedure called transcatheter aortic valve replacement (TAVR) to replace a narrowed aortic valve. TAVR may be an option for people who are considered to be at intermediate or high risk of complications from surgical aortic valve replacement.
In TAVR, doctors insert a catheter in your leg or chest and guide it to your heart. A replacement valve is then inserted through the catheter and guided to your heart. A balloon may expand the valve, or some valves can self-expand. When the valve is implanted, doctors remove the catheter from your blood vessel.
Doctors may also conduct a catheter procedure to insert a replacement valve into a failing biological tissue valve that is no longer working properly. Other catheter procedures to repair or replace aortic valves continue to be researched.
Lifestyle and home remedies
You’ll have regular follow-up appointments with your doctor to monitor your condition. You’ll need to continue taking all your medications as prescribed.
Your doctor may suggest you incorporate several heart-healthy lifestyle changes into your life, including:
- Eating a heart-healthy diet. Eat a variety of fruits and vegetables, low-fat or fat-free dairy products, poultry, fish, and whole grains. Avoid saturated and trans fat, and excess salt and sugar.
- Maintaining a healthy weight. Aim to keep a healthy weight. If you’re overweight or obese, your doctor may recommend that you lose weight.
- Getting regular physical activity. Aim to include about 30 minutes of physical activity, such as brisk walks, into your daily fitness routine.
- Managing stress. Find ways to help manage your stress, such as through relaxation activities, meditation, physical activity, and spending time with family and friends.
- Avoiding tobacco. If you smoke, quit. Ask your doctor about resources to help you quit smoking. Joining a support group may be helpful.
For women with aortic valve stenosis, it’s important to talk with your doctor before you become pregnant. Your doctor can discuss with you which medications you can safely take, and whether you may need a procedure to treat your valve condition prior to pregnancy.
You’ll likely require close monitoring by your doctor during pregnancy. Doctors may recommend that women with severe valve stenosis avoid pregnancy to avoid the risk of complications.
Long-term outlook