Hydrocephalus is the buildup of fluid in the cavities (ventricles) deep within the brain. The excess fluid increases the size of the ventricles and puts pressure on the brain. Cerebrospinal fluid normally flows through the ventricles and bathes the brain and spinal column. But the pressure of too much cerebrospinal fluid associated with hydrocephalus can damage brain tissues and cause a range of impairments in brain function. Hydrocephalus can happen at any age, but it occurs more frequently among infants and adults 60 and over. Surgical treatment for hydrocephalus can restore and maintain normal cerebrospinal fluid levels in the brain. Many different therapies are often required to manage symptoms or functional impairments resulting from hydrocephalus.
Symptoms
The signs and symptoms of hydrocephalus vary somewhat by age of onset.
Infants
Common signs and symptoms of hydrocephalus in infants include:
Changes in the head
- An unusually large head
- A rapid increase in the size of the head
- A bulging or tense soft spot (fontanel) on the top of the head
Physical signs and symptoms
- Vomiting
- Sleepiness
- Irritability
- Poor feeding
- Seizures
- Eyes fixed downward (sunsetting of the eyes)
- Deficits in muscle tone and strength
- Poor responsiveness to touch
- Poor growth
Toddlers and older children
Among toddlers and older children, signs and symptoms may include:
Physical signs and symptoms
- Headache
- Blurred or double vision
- Eyes fixed downward (sunsetting of eyes)
- Abnormal enlargement of a toddler’s head
- Sleepiness or lethargy
- Nausea or vomiting
- Unstable balance
- Poor coordination
- Poor appetite
- Seizures
- Urinary incontinence
Behavioral and cognitive changes
- Irritability
- Change in personality
- Decline in school performance
- Delays or problems with previously acquired skills, such as walking or talking
Young and middle-aged adults
Common signs and symptoms in this age group include:
- Headache
- Lethargy
- Loss of coordination or balance
- Loss of bladder control or a frequent urge to urinate
- Impaired vision
- Decline in memory, concentration and other thinking skills that may affect job performance
Older adults
Among adults 60 years of age and older, the more common signs and symptoms of hydrocephalus are:
- Loss of bladder control or a frequent urge to urinate
- Memory loss
- Progressive loss of other thinking or reasoning skills
- Difficulty walking, often described as a shuffling gait or the feeling of the feet being stuck
- Poor coordination or balance
When to see a doctor
Seek emergency medical care for infants and toddlers experiencing these signs and symptoms:
- A high-pitched cry
- Problems with sucking or feeding
- Unexplained, recurrent vomiting
- An unwillingness to move the head or lay down
- Breathing difficulties
- Seizures
Diagnosis
A diagnosis of hydrocephalus is usually based on:
- Your answers to the doctor’s questions about signs and symptoms
- A general physical
- A neurological exam
- Brain imaging tests
Neurological exam
The type of neurological exam will depend on a person’s age. The neurologist may ask questions and conduct relatively simple tests in the office to judge muscle condition, movement, well-being and how well the senses are functioning.
Brain imaging
Brain imaging tests can show enlarged ventricles caused by excess cerebrospinal fluid. They may also be used to identify underlying causes of hydrocephalus or other conditions contributing to the symptoms. Imaging tests may include:
- Ultrasound. Ultrasound imaging, which uses high-frequency sound waves to produce images, is often used for an initial assessment for infants because it’s a relatively simple, low-risk procedure. The ultrasound device is placed over the soft spot (fontanel) on the top of a baby’s head. Ultrasound may also detect hydrocephalus prior to birth when the procedure is used during routine prenatal examinations.
- Magnetic resonance imaging (MRI) uses radio waves and a magnetic field to produce detailed 3-D or cross-sectional images of the brain. This test is painless, but it is noisy and requires lying still.Children may need mild sedation for some MRI scans. However, some hospitals use a very fast version of MRI that generally doesn’t require sedation.
- Computerized tomography (CT) scan is a specialized X-ray technology that can produce cross-sectional views of the brain. Scanning is painless and quick. But this test also requires lying still, so a child usually receives a mild sedative.Drawbacks to CT scanning include less detailed images than an MRI, and exposure to a small amount of radiation. CT scans for hydrocephalus are usually used only for emergency exams.
Treatment
One of two surgical treatments may be used to treat hydrocephalus.
1. Shunt
-
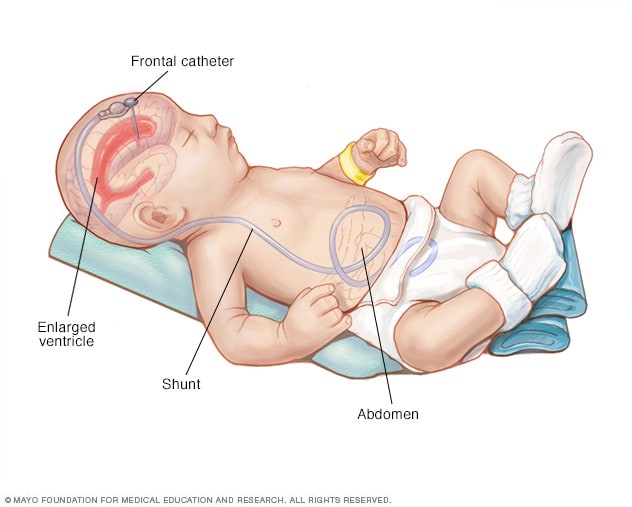
Shunt system
The most common treatment for hydrocephalus is the surgical insertion of a drainage system, called a shunt. It consists of a long, flexible tube with a valve that keeps fluid from the brain flowing in the right direction and at the proper rate.
One end of the tubing is usually placed in one of the brain’s ventricles. The tubing is then tunneled under the skin to another part of the body where the excess cerebrospinal fluid can be more easily absorbed — such as the abdomen or a chamber in the heart.
People who have hydrocephalus usually need a shunt system for the rest of their lives, and regular monitoring is required.
2. Endoscopic third ventriculostomy
Endoscopic third ventriculostomy is a surgical procedure that can be used for some people. In the procedure, your surgeon uses a small video camera to have direct vision inside the brain. Your surgeon makes a hole in the bottom of one of the ventricles or between the ventricles to enable cerebrospinal fluid to flow out of the brain.
Complications of surgery
Both surgical procedures can result in complications. Shunt systems can stop draining cerebrospinal fluid or poorly regulate drainage because of mechanical malfunctions, blockage or infections. Complications of ventriculostomy include bleeding and infections.
Any failure requires prompt attention, surgical revisions or other interventions. Signs and symptoms of problems may include:
- Fever
- Irritability
- Drowsiness
- Nausea or vomiting
- Headache
- Vision problems
- Redness, pain or tenderness of the skin along the path of the shunt tube
- Abdominal pain when the shunt valve is in the abdomen
- Recurrence of any of the initial hydrocephalus symptoms
Other treatments
Some people with hydrocephalus, particularly children, may need additional treatment, depending on the severity of long-term complications of hydrocephalus.
A care team for children may include a:
- Pediatrician or psychiatrist, who oversees the treatment plan and medical care
- Pediatric neurologist, who specializes in the diagnosis and treatment of neurological disorders in children
- Occupational therapist, who specializes in therapy to develop everyday skills
- Developmental therapist, who specializes in therapy to help your child develop age-appropriate behaviors, social skills and interpersonal skills
- Mental health provider, such as a psychologist or psychiatrist
- Social worker, who assists the family with accessing services and planning for transitions in care
- Special education teacher, who addresses learning disabilities, determines educational needs and identifies appropriate educational resources