Influenza, commonly called “the flu,” is an illness caused by RNA viruses (Orthomyxoviridae family) that infect the respiratory tract of many animals, birds, and humans.(nose, throat and lungs.) but it’s not the same as stomach “flu” viruses that cause diarrhea and vomiting.For most people, the flu resolves on its own. But sometimes, influenza and its complications can be deadly.
Risk of developing flu complications include:
- Young children under age 5, and especially those under 6 months
- Adults older than age 65
- Residents of nursing homes and other long-term care facilities
- Pregnant women and women up to two weeks after giving birth
- People with weakened immune systems
- Native Americans
- People who have chronic illnesses, such as asthma, heart disease, kidney disease, liver disease and diabetes
- People who are very obese, with a body mass index (BMI) of 40 or higher
Though the annual influenza vaccine isn’t 100% effective, it’s still your best defense against the flu.
Symptoms

At first, the flu may seem like a common cold with a runny nose, sneezing and sore throat. But colds usually develop slowly, whereas the flu tends to come on suddenly. And although a cold can be a bother, you usually feel much worse with the flu.
Common signs and symptoms of the flu include:
- Fever
- Aching muscles
- Chills and sweats
- Headache
- Dry, persistent cough
- Shortness of breath
- Tiredness and weakness
- Runny or stuffy nose
- Sore throat
- Eye pain
- Vomiting and diarrhea, but this is more common in children than adults
If you have emergency signs and symptoms of the flu, get medical care right away. For adults, emergency signs and symptoms can include:
- Difficulty breathing or shortness of breath
- Chest pain
- Ongoing dizziness
- Seizures
- Worsening of existing medical conditions
- Severe weakness or muscle pain
Emergency signs and symptoms in children can include:
- Difficulty breathing
- Blue lips
- Chest pain
- Dehydration
- Severe muscle pain
- Seizures
- Worsening of existing medical conditions
Diagnosing Flu
Some of the symptoms of flu and COVID-19 are similar, making it hard to tell the difference between them based on symptoms alone. Diagnostic testing can help determine if you are sick with the flu or COVID-19.
Medical professionals clinically diagnose the flu by evaluating the patient’s history of association with people known to have the disease and their symptoms listed above. Usually, a health care professional performs a quick test (for example, nasopharyngeal swab sample) to see if the patient has an influenza A or B viral infection. Most of the tests can distinguish between A and B types.
A number of flu tests are available to detect influenza viruses in respiratory specimens. The most common are called “rapid influenza diagnostic tests (RIDTs).” RIDTs work by detecting the parts of the virus (antigens) that stimulate an immune response. These tests can provide results within approximately 10-15 minutes but are not as accurate as other flu tests. Therefore, you could still have flu, even though your rapid test result is negative. Other flu tests are called “rapid molecular assays” that detect genetic material of the virus. Rapid molecular assays produce results in 15-20 minutes and are more accurate than RIDTs. In addition, there are several more accurate and sensitive flu tests available that must be performed in specialized laboratories, such as those found in hospitals or state public health laboratories. All of these tests require that a health care provider swipe the inside of your nose or the back of your throat with a swab and then send the swab for testing. Results may take one to several hours
How long is the flu contagious?
The flu is typically contagious about 24-48 hours before symptoms appear (from about the last day of the incubation period) and in normal healthy adults is contagious for another 5-7 days. Children are usually contagious for a little while longer (about 7-10 days). Individuals with severe infections may be contagious as long as symptoms last (about 7-14 days).
Complications
If you’re young and healthy, the flu usually isn’t serious. Although you may feel miserable while you have it, the flu usually goes away in a week or two with no lasting effects. But children and adults at high risk may develop complications that may include:
- Pneumonia
- Bronchitis
- Asthma flare-ups
- Heart problems
- Ear infections
- Acute respiratory distress syndrome
Pneumonia is one of the most serious complications. For older adults and people with a chronic illness, pneumonia can be deadly.
Types of Influenza Viruses
There are four types of influenza viruses: A, B, C and D. Human influenza A and B viruses cause seasonal epidemics of disease (known as the flu season) almost every winter in the United States. Influenza A viruses are the only influenza viruses known to cause flu pandemics, i.e., global epidemics of flu disease. A pandemic can occur when a new and very different influenza A virus emerges that both infects people and has the ability to spread efficiently between people. Influenza type C infections generally cause mild illness and are not thought to cause human flu epidemics. Influenza D viruses primarily affect cattle and are not known to infect or cause illness in people.
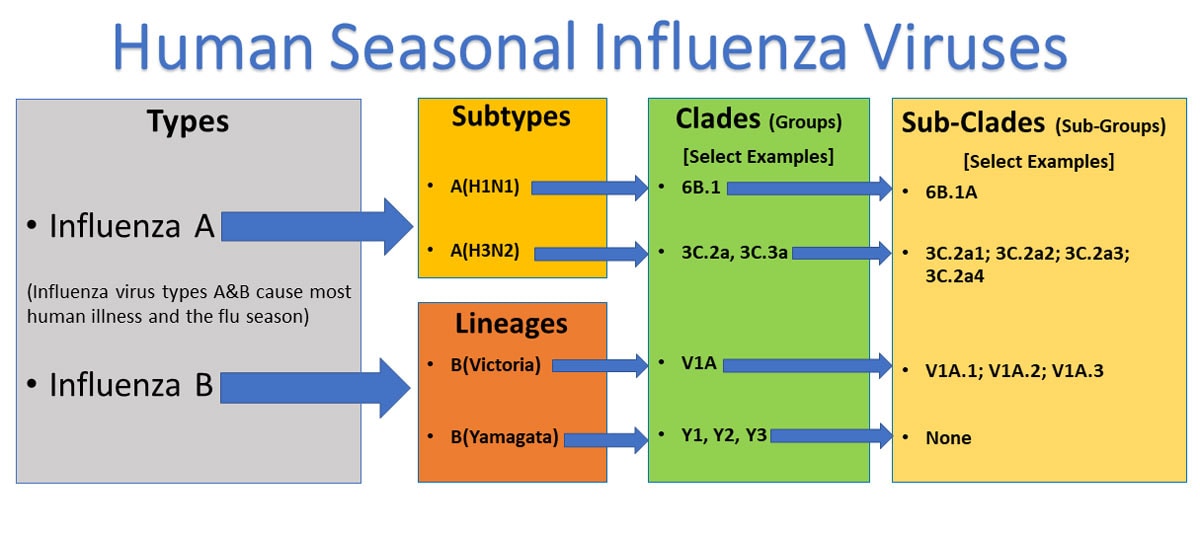
Influenza A viruses are divided into subtypes based on two proteins on the surface of the virus: hemagglutinin (H) and neuraminidase (N). There are 18 different hemagglutinin subtypes and 11 different neuraminidase subtypes (H1 through H18 and N1 through N11, respectively). While there are potentially 198 different influenza A subtype combinations, only 131 subtypes have been detected in nature. Current subtypes of influenza A viruses that routinely circulate in people include: A(H1N1) and A(H3N2). Influenza A subtypes can be further broken down into different genetic “clades” and “sub-clades.” See the “Influenza Viruses” graphic below for a visual depiction of these classifications.
This graphic shows the two types of influenza viruses (A,B) that cause most human illness and that are responsible for the flu season each year. Influenza A viruses are further classified into subtypes, while influenza B viruses are further classified into two lineages: B/Yamagata and B/Victoria. Both influenza A and B viruses can be further classified into specific clades and sub-clades (which are sometimes called groups and sub-groups).
Flu Treatment and Prevention
If you get sick with flu, antiviral drugs may be a treatment option.
Check with your doctor promptly if you are at high risk of serious flu complications and you get flu symptoms. People at high risk of flu complications include young children, adults 65 years of age and older, pregnant women, and people with certain medical conditions such as asthma, diabetes and heart disease.
When used for treatment, antiviral drugs can lessen symptoms and shorten the time you are sick by 1 or 2 days. They also can prevent serious flu complications, like pneumonia. For people at high risk of serious flu complications, treatment with antiviral drugs can mean the difference between milder or more serious illness possibly resulting in a hospital stay. CDC recommends prompt treatment for people who have influenza infection or suspected influenza infection and who are at high risk of serious flu complications.
Annual influenza vaccination can prevent most of the illness and death that influenza causes. The CDC’s current Advisory Committee on Immunization Practices (ACIP) issued recommendations for everyone 6 months of age and older, who do not have any contraindications to vaccination, to receive a flu vaccine each year.
Flu vaccine (influenza vaccine made from inactivated and sometimes attenuated [noninfective] virus or virus components) is specifically recommended for those who are at high risk for developing serious complications from influenza infection.
Other simple hygiene methods can reduce or prevent some individuals from getting the flu. For example, avoiding kissing, handshakes, and sharing drinks or food with infected people and avoiding touching surfaces like sinks and other items handled by individuals with the flu are good preventive measures. Washing one’s hands with soap and water or by using an alcohol-based hand sanitizer frequently during the day may help prevent the infection. Individuals with the flu should avoid coughing or sneezing on uninfected people; quick hugs are probably okay as long as there is no contact with mucosal surfaces and/or droplets that may contain the virus. Wearing a mask may help reduce your chances of getting the disease, and if you unknowingly or know you have the infection, help to reduce spreading it to others
Controlling the spread of infection
The influenza vaccine isn’t 100% effective, so it’s also important to take several measures to reduce the spread of infection, including:
- Wash your hands. Washing your hands often with soap and water for at least 20 seconds is an effective way to prevent many common infections. Or use alcohol-based hand sanitizers if soap and water aren’t available.
- Avoid touching your face. Avoid touching your eyes, nose and mouth.
- Cover your coughs and sneezes. Cough or sneeze into a tissue or your elbow. Then wash your hands.
- Clean surfaces. Regularly clean often-touched surfaces to prevent spread of infection from touching a surface with the virus on it and then your face.
- Avoid crowds. The flu spreads easily wherever people gather — in child care centers, schools, office buildings, auditoriums and public transportation. By avoiding crowds during peak flu season, you reduce your chances of infection.Also avoid anyone who is sick. And if you’re sick, stay home for at least 24 hours after your fever is gone so that you lessen your chance of infecting others.
Takeaway
Influenza viruses travel through the air in droplets when someone with the infection coughs, sneezes or talks. You can inhale the droplets directly, or you can pick up the germs from an object — such as a telephone or computer keyboard — and then transfer them to your eyes, nose or mouth.
People with the virus are likely contagious from about a day before symptoms appear until about five days after they start. Children and people with weakened immune systems may be contagious for a slightly longer time.
During the COVID -19 pandemic, both COVID -19 and the flu may be spreading at the same time. Your local health practioner may help and suggest other precautions to reduce your risk of COVID -19 or the flu. For example, you may need to practice social distancing (physical distancing) and stay at least 6 feet (2 meters) from others outside your household. You may also need to wear a cloth face mask when around people outside your household.